Efecto de las condiciones individuales, del hogar y del área de residencia en la autopercepción de su salud en adultos colombianos: un estudio multinivel
Resumen
Introducción. La autopercepción de la salud se asocia con la morbilidad y la mortalidad debido principalmente al efecto de las condiciones individuales y las características sociales y del ambiente en el que viven las personas.
Objetivo. Investigar los factores individuales, del hogar y de la localidad asociados con la autopercepción de la salud en adultos colombianos.
Materiales y métodos. Se llevó a cabo un estudio transversal. La información sobre las 19 localidades urbanas consideradas se obtuvo de bases de datos nacionales, en tanto que los datos sobre los 37.352 individuos anidados en 15.788 hogares provinieron de una encuesta de base poblacional. Dada la estructura jerárquica de los datos, las estimaciones del efecto de las variables individuales, del hogar y de la localidad sobre la autopercepción de la salud se hicieron utilizando un modelo de regresión logística de tres niveles.
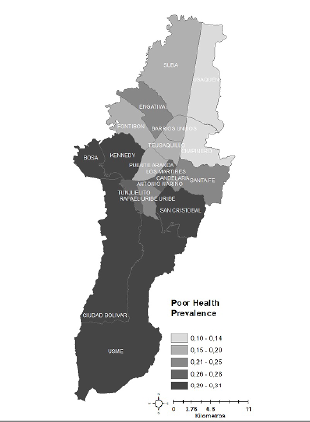
Resultados. Los modelos multinivel ajustados evidenciaron que a nivel individual había una mayor probabilidad de tener una peor percepción de la salud entre adultos
mayores, personas de bajo nivel socioeconómico, sin compañero, físicamente inactivos y con enfermedades. A nivel de hogar, la peor percepción de la salud se asoció con la pertenencia a familias de bajo nivel socioeconómico, residentes cerca de fábricas, áreas contaminadas, inseguras y de alto ruido. Por último, a nivel de localidad y después del ajuste por variables individuales y del hogar, la residencia en localidades pobres aumentó la probabilidad de tener una peor percepción de la propia salud.
Conclusiones. Los resultados evidencian la necesidad de considerar un marco conceptual más amplio en el momento de diseñar e implementar estrategias y programas que apunten al mejoramiento de las condiciones de salud de las poblaciones urbanas en Latinoamérica.
Descargas
Referencias bibliográficas
Alazraqui M, Diez Roux A V, Fleischer N, Spinelli H. Self-rated health and social inequalities, Buenos Aires, Argentina, 2005. Cad Saúde Pública. 2009;25:1990-2000. https://doi.org/10.1590/S0102-311X2009000900013
Velarde-Jurado E, Avila-Figueroa C. Evaluation of the quality of life. Salud Pública Mex. 2002;44:349-61.
Agyemang C, van Hooijdonk C, Wendel-Vos W, Lindeman E, Stronks K, Droomers M. The association of neighbourhood psychosocial stressors and self-rated health in Amsterdam, The Netherlands. J Epidemiol Community Health. 2007;61:1042-9. https://doi.org/10.1136/jech.2006.052548
Heistaro S, Jousilahti P, Lahelma E, Vartiainen E, Puska P. Self-rated health and mortality: A long term prospective study in eastern Finland. J Epidemiol Community Health. 2001;55:227-32. https://doi.org/10.1136/jech.55.4.227
Idler EL, Angel RJ. Self-rated health and mortality in the NHANES-I Epidemiologic Follow-up Study. Am J Public Heal. 1990;80:446-52. https://doi.org/10.2105/AJPH.80.4.446
Idler EL, Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. J Health Soc Behav. 1997;38:21-37.
Idler EL, Kasl S V, Lemke JH. Self-evaluated health and mortality among the elderly in New Haven, Connecticut, and Iowa and Washington counties, Iowa, 1982-1986. Am J Epidemiol. 1990;131:91-103. https://doi.org/10.1093/oxfordjournals.aje.a115489
Mossey JM, Shapiro E. Self-rated health: A predictor of mortality among the elderly. Am J Public Health. 1982;72:800-8. https://doi.org/10.2105/AJPH.72.8.800
Benavides FG, Benach J, Diez-Roux A V, Roman C. How do types of employment relate to health indicators? Findings from the second European survey on working conditions. J Epidemiol Community Health. 2000;54:494-501. https://doi.org/10.1136/jech.54.7.494
Benyamini Y, Leventhal EA, Leventhal H. Gender differences in processing information for making self-assessments of health. Psychosom Med. 2000;62:354-64.
Dachs JN. Factors determining inequalities in the health condition self-assessment in Brazil: Analysis of data of PNAD/1998. Cien Saúde Colet. 2002;7:641-57.
Heistaro S, Laatikainen T, Vartiainen E, Puska P, Uutela A, Pokusajeva S, et al. Self-reported health in the Republic of Karelia, Russia and in north Karelia, Finland in 1992. Eur J Public Health. 2001;11:74-80. https://doi.org/10.1093/eurpub/11.1.74
Mansyur C, Amick BC, Harrist RB, Franzini L. Social capital, income inequality, and self-rated health in 45 countries. Soc Sci Med. 2008;66:43-56. https://doi.org/10.1016/j.socscimed.2007.08.015
Kawachi I, Subramanian SV. Neighbourhood influences on health. J Epidemiol Community Health. 2007;61:3-4. https://doi.org/10.1136/jech.2005.045203
Macintyre S, Ellaway A, Cummins S. Place effects on health: How can we conceptualise, operationalise and measure them? Soc Sci Med. 2002;55:125-39.
Cremonese C, Backes V, Olinto MT, Dias-da-Costa JS, Pattussi MP. Neighborhood sociodemographic and environmental contexts and self-rated health among Brazilian adults: A multilevel study. Cad Saúde Pública. 2010;26:2368-78. https://doi.org/10.1590/S0102-311X2010001200015
Cummins S, Stafford M, Macintyre S, Marmot M, Ellaway A. Neighbourhood environment and its association with self rated health: Evidence from Scotland and England. J Epidemiol Community Health. 2005;59:207-13. https://doi.org/10.1136/jech.2003.016147
Diez Roux AV, Am JP. Investigating neighborhood and area effects on health. Am J Public Health. 2001;91:1783-9. https://doi.org/10.2105/ajph.91.11.1783
Diez Roux AV. Neighborhoods and health: Where are we and where do we go from here? Rev Epidemiol Santé Publique. 2007;55:13-21.
Pampalon R, Hamel D, De Koninck M, Disant MJ. Perception of place and health: Differences between neighbourhoods in the Quebec City region. Soc Sci Med. 2007;65:95-111. https://doi.org/10.1016/j.socscimed.2007.02.044
Patel K V, Eschbach K, Rudkin LL, Peek MK, Markides KS. Neighborhood context and self-rated health in older Mexican Americans. Ann Epidemiol. 2003;13:620-8.
https://doi.org/10.1016/S1047-2797(03)00060-7
Poortinga W, Dunstan FD, Fone DL. Neighbourhood deprivation and self-rated health: The role of perceptions of the neighbourhood and of housing problems. Health Place. 2008;14:562-75. https://doi.org/10.1016/j.healthplace.2007.10.003
Poortinga W, Dunstan FD, Fone DL. Perceptions of the neighbourhood environment and self rated health: A multilevel analysis of the Caerphilly Health and Social Needs Study. BMC Public Health. 2007;7:285. https://doi.org/10.1186/1471-2458-7-285
Mrug S, Windle M. Mediators of neighborhood influences on externalizing behavior in preadolescent children. J Abnorm Child Psychol. 2009;37:265-80. https://doi.org/10.1007/s10802-008-9274-0
Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: A multilevel study of collective efficacy. Science. 1997;277:918-24. https://doi.org/10.1126/science.277.5328.918
Reijneveld SA, Verheij RA, De Bakker DH. The impact of area deprivation on differences in health: Does the choice of the geographical classification matter? J Epidemiol Community Health. 2000;54:306-13. https://doi.org/10.1136/jech.54.4.306
Reijneveld SA. Neighbourhood socioeconomic context and self reported health and smoking: A secondary analysis of data on seven cities. J Epidemiol Community Health. 2002;56:935-42. https://doi.org/10.1136/jech.56.12.935
Wen M, Browning CR, Cagney KA. Poverty, affluence, and income inequality: Neighborhood economic structure and its implications for health. Soc Sci Med. 2003;57:843-60. https://doi.org/10.1016/S0277-9536(02)00457-4
29. Franzini L, Caughy M, Spears W, Fernández-Esquer ME. Neighborhood economic conditions, social processes, and self-rated health in low-income neighborhoods in Texas: A multilevel latent variables model. Soc Sci Med. 2005;61:1135-50. https://doi.org/10.1016/j.socscimed.2005.02.010
Stafford M, Marmot M. Neighbourhood deprivation and health: Does it affect us all equally? Int J Epidemiol. 2003;32:357-66. https://doi.org/10.1093/ije/dyg084
Steptoe A, Feldman PJ. Neighborhood problems as sources of chronic stress: Development of a measure of neighborhood problems, and associations with socioeconomic status and health. Ann Behav Med. 2001;23:177–85. https://doi.org/10.1207/S15324796ABM2303_5
Wong IO, Cowling BJ, Lo S V, Leung GM. A multilevel analysis of the effects of neighbourhood income inequality on individual self-rated health in Hong Kong. Soc Sci Med. 2009;68:124-32. https://doi.org/10.1016/j.socscimed.2008.09.064
Diez Roux AV. A glossary for multilevel analysis. J Epidemiol Community Health. 2002;56:588-94. https://doi.org/10.1136/jech.56.8.588
Diez-Roux AV. Multilevel analysis in public health research. Annu Rev Public Health. 2000;21:171-92. https://doi.org/10.1146/annurev.publhealth.21.1.171
Duncan C, Jones K, Moon G. Context, composition and heterogeneity: Using multilevel models in health research. Soc Sci Med. 1998;46:97-117. https://doi.org/10.1016/S0277-9536(97)00148-2
Santos SM, Chor D, Werneck GL, Coutinho ES. Association between contextual factors and self-rated health: A systematic review of multilevel studies. Cad Saúde Pública. 2007;23:2533-54. https://doi.org/10.1590/S0102-311X200700110000
Departamento Administrativo Nacional de Estadística. Encuesta Multipropósito para Bogotá Distrito Capital: EMB 2011 Información general. Accessed: March 13, 2018. Available from: http://microdatos.dane.gov.co/index.php/catalog/189/related_materials
Alcaldía Mayor Santa Fé de Bogotá. Encuesta Multipropósito para Bogotá EMB 2011-2014. Accessed: March 13, 2018. Available from: http://www.sdp.gov.co/sites/default/files/presentacion_03_febre_2016.pdf
Diez-Roux AV, Link BG, Northridge ME. A multilevel analysis of income inequality and cardiovascular disease risk factors. Soc Sci Med. 2000;50:673-87. https://doi.org/10.1016/S0277-9536(99)00320-2
Alcaldía Mayor Santa Fé de Bogotá. Indicadores de pobreza. Encuesta multipropósito. Bogotá D.C.: Alcaldía Mayor; 2011.
Victora CG, Huttly SR, Fuchs SC, Olinto MT. The role of conceptual frameworks in epidemiological analysis: A hierarchical approach. Int J Epidemiol. 1997;26:224-7. https://doi.org/10.1093/ije/26.1.224
Merlo J, Chaix B, Ohlsson H, Beckman A, Johnell K, Hjerpe P, et al. A brief conceptual tutorial of multilevel analysis in social epidemiology: Using measures of clustering in multilevel logistic regression to investigate contextual phenomena. J Epidemiol Community Health. 2006;60:290-7. https://doi.org/10.1136/jech.2004.029454
Larsen K, Merlo J. Appropriate assessment of neighborhood effects on individual health: Integrating random and fixed effects in multilevel logistic regression. Am J Epidemiol. 2005;161:81-8. https://doi.org/10.1093/aje/kwi017
Jones K, Subramanian S. Developing multilevel models for analysing contextuality, heterogeneity and change. Volume 1. Boston MA: University of Bristol; 2013.
Mickey RM, Greenland S. The impact of confounder selection criteria on effect estimation. Am J Epidemiol. 1989;129:125-37. https://doi.org/10.1093/oxfordjournals.aje.a115101
Maldonado G, Greenland S. Simulation study of confounder-selection strategies. Am J Epidemiol. 1993;138:923-36. https://doi.org/10.1093/oxfordjournals.aje.a116813
Spiegelhalter DJ, Best NG, Carlin BP, Van Der Linde A. Bayesian measures of model complexity and fit. J R Stat Soc Ser B Stat Methodol. 2002;64:583-639.
Leckie G, Charlton C. runmlwin : A Program to Run the MLwiN Multilevel Modeling Software from within Stata. J Stat Softw. 2015;52:1-40.
Draper D. Bayesian Multilevel Analysis and MCMC. In: Leeuw J., Meijer E, editors. Handbook of Multilevel Analysis. New York, NY: Springer: 2008.
Rasbash J, Steele F, Browne WJ, Goldstein H, Charlton CMJ. A User ’ s Guide to MLwiN, v2.26. Centre for Multilevel Modelling. Bristol: University of Bristol; 2012.
Tay JB, Kelleher CC, Hope A, Barry M, Gabhainn SN, Sixsmith J. Influence of sociodemographic and neighbourhood factors on self-rated health and quality of life in rural communities: Findings from the agriproject in the Republic of Ireland. J Epidemiol Community Health. 2004;58:904-11. https://doi.org/10.1136/jech.2002.006643
Stafford M, Cummins S, Macintyre S, Ellaway A, Marmot M. Gender differences in the associations between health and neighbourhood environment. Soc Sci Med. 2005;60:1681-92. https://doi.org/10.1016/j.socscimed.2004.08.028
Algunos artículos similares:
- Elizabeth Borrero, Gabriel Carrasquilla, Neal Alexander, Descentralización y reforma: ¿cuál es su impacto sobre la incidencia de malaria en los municipios colombianos? , Biomédica: Vol. 32 (2012): Suplemento 1, Malaria
- Raúl Murillo, Ricardo Cendales, Carolina Wiesner, Marion Piñeros, Sandra Tovar, Efectividad de la citología cérvico-uterina para la detección temprana de cáncer de cuello uterino en el marco del sistema de salud de Colombia , Biomédica: Vol. 29 Núm. 3 (2009)
- Sandra Lorena Girón, Julio César Mateus, Fabián Méndez, Impacto de un botadero a cielo abierto en el desarrollo de síntomas respiratorios y en costos familiares de atención en salud de niños entre 1 y 5 años en Cali, Colombia , Biomédica: Vol. 29 Núm. 3 (2009)
- José Joaquín Carvajal, Ligia Inés Moncada, Mauricio Humberto Rodríguez, Ligia del Pilar Pérez, Víctor Alberto Olano, Caracterización preliminar de los sitios de cría de Aedes (Stegomyia) albopictus (Skuse, 1894) (Diptera: Culicidae) en el municipio de Leticia, Amazonas, Colombia , Biomédica: Vol. 29 Núm. 3 (2009)
- Andrés Páez, Gloria Rey, Carlos Agudelo, Alvaro Dulce, Edgar Parra, Hernando Díaz-Granados, Damaris Heredia, Luis Polo, Brote de rabia urbana transmitida por perros en el distrito de Santa Marta, Colombia, 2006-2008 , Biomédica: Vol. 29 Núm. 3 (2009)
- Patricia Escobar, Katherine Paola Luna, Indira Paola Hernández, César Mauricio Rueda, María Magdalena Zorro, Simon L. Croft, Susceptibilidad in vitro a hexadecilfosfocolina (miltefosina), nifurtimox y benznidazole de cepas de Trypanosoma cruzi aisladas en Santander, Colombia , Biomédica: Vol. 29 Núm. 3 (2009)
- Gustavo Pradilla, Julio César Mantilla, Reynaldo Badillo, Encefalitis rábica humana por mordedura de murciélago en un área urbana de Colombia , Biomédica: Vol. 29 Núm. 2 (2009)
- Mauricio Beltrán, María Cristina Navas, María Patricia Arbeláez, Jorge Donado, Sergio Jaramillo, Fernando De la Hoz, Cecilia Estrada, Lucía del Pilar Cortés, Amalia de Maldonado, Gloria Rey, Seroprevalencia de infección por virus de la hepatitis B y por virus de la inmunodeficiencia humana en una población de pacientes con múltiples transfusiones en cuatro hospitales, Colombia, Sur América , Biomédica: Vol. 29 Núm. 2 (2009)
- Rosa Magdalena Uscátegui, Adriana M. Correa, Jaime Carmona-Fonseca, Cambios en las concentraciones de retinol, hemoglobina y ferritina en niños palúdicos colombianos , Biomédica: Vol. 29 Núm. 2 (2009)
- Claudia M.E. Romero-Vivas, Luis Eduardo Castro, Lila Visbal, Ana María Santos, Esther Díaz, Miasis cutánea por Cochliomyia hominivorax (Coquerel) (Díptera: Calliphoridae) en el Hospital Universidad del Norte, Soledad, Atlántico , Biomédica: Vol. 29 Núm. 1 (2009)
| Estadísticas de artículo | |
|---|---|
| Vistas de resúmenes | |
| Vistas de PDF | |
| Descargas de PDF | |
| Vistas de HTML | |
| Otras vistas | |

























