Cost-utility analysis of an implantable cardioverterdefibrillator for the treatment of patients with ischemic or non-ischemic New York Heart Association class II or III heart failure in Colombia
Abstract
Introduction: The use of an implantable cardioverter-defibrillator reduces the probability of sudden cardiac death in patients with heart failure.
Objective: To determine the cost-utility relationship of an implantable cardioverter-defibrillator compared to optimal pharmacological therapy for patients with ischemic or non-ischemic New York Heart Association class II or III (NYHA II-III) heart failure in Colombia.
Materials and methods: We developed a Markov model including costs, effectiveness, and quality of life from the perspective of the Colombian health system. For the baseline case, we adopted a time horizon of 10 years and discount rates of 3% for costs and 3.5% for benefits.
The transition probabilities were obtained from a systematic review of the literature. The outcome used was the quality-adjusted life years. We calculated the costs by consulting with the manufacturers of the device offered in the Colombian market and using national-level pricing manuals. We conducted probabilistic and deterministic sensitivity analyses.
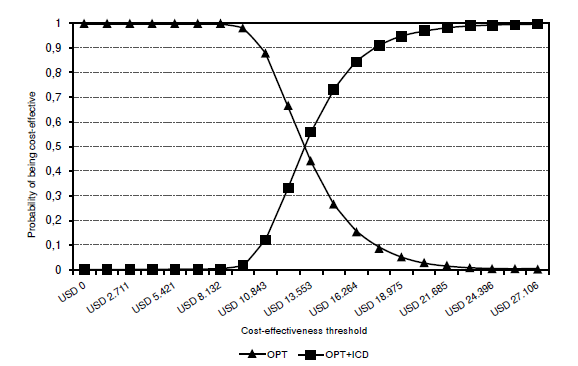
Results: In the base case, the incremental cost-effectiveness ratio for the implantable cardioverter-defibrillator was USD$ 13,187 per quality-adjusted life year gained. For a willingness-to-pay equivalent to three times the gross domestic product per capita as a reference (USD$ 19,139 in 2017), the device would be a cost-effective strategy for the Colombian health system. However, the result may change according to the time horizon, the probability of death, and the price of the device.
Conclusions: The use of an implantable cardioverter-defibrillator for preventing sudden cardiac death in patients with heart failure would be a cost-effective strategy for Colombia. The results should be examined considering the uncertainty.
Downloads
References
McMurray JJ, Petrie MC, Murdoch DR, Davie AP. Clinical epidemiology of heart failure: Public and private health burden. Eur Heart J. 1998;19:9-16.
Ziaeian B, Fonarow GC. Epidemiology and aetiology of heart failure. Nat Rev Cardiol. 2016;13:368-78. https://doi.org/10.1038/nrcardio.2016.25
Berry C, Murdoch DR, McMurray JJ. Economics of chronic heart failure. Eur J Heart Fail. 2001;3:283-291. https://doi.org/10.1016/S1388-9842(01)00123-4
Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics: 2015 update: A report from the American Heart Association Statistics Committee and Stroke Statistics. Circulation. 2015;131:29-322. https://doi.org/10.1161/CIR.0000000000000152
Bui AL, Horwich TB, Fonarow GC. Epidemiology and risk profile of heart failure. Nat Rev Cardiol. 2011;8:30-41. https://doi.org/10.1038/nrcardio.2010.165
Tamayo D, Rodríguez V, Rojas M, Rincón M, Franco C, Ibarra M, et al. Costos ambulatorios y hospitalarios de la falla cardiaca en dos hospitales de Bogotá. Acta Médica Colombiana. 2013;38:208-12.
Haas G, Abraham W. Comprehensive pharmacologic management strategies for heart failure. In: Yu C, Hayes D, Auricchio A, editors. Cardiac resynchronization therapy. Massachusetts: Blackwell; 2008. p. 15-34.
Theuns DA, Smith T, Hunink MG, Bardy GH, Jordaens L. Effectiveness of prophylactic implantation of cardioverter-defibrillators without cardiac resynchronization therapy in patients with ischaemic or non-ischaemic heart disease: A systematic review and metaanalysis. Europace. 2010;12:1564-1570. https://doi.org/10.1093/europace/euq329
Ezekowitz JA, Rowe BH, Dryden DM, Hooton N, Vandermeer B, Spooner C, et al. Systematic review: Implantable cardioverter defibrillators for adults with left ventricular systolic dysfunction. Ann Intern Med. 2007;147:251-262. https://doi.org/10.7326/0003-4819-147-4-200708210-00007
Ministerio de la Protección Social, Colciencias, Centro de Estudios e Investigación en Salud de la Fundación Santa Fe de Bogotá, Escuela de Salud Pública de la Universidad de Harvard. Guía metodológica para el desarrollo de Guías de atención integral en el Sistema General de Seguridad Social en Salud Colombiano. Accessed on: October 1, 2018. Available at: https://www.minsalud.gov.co/salud/Documents/Gu%C3%ADa%20Metodol%C3%B3gica%20para%20la%20elaboraci%C3%B3n%20de%20gu%C3%ADas.pdf
Ministerio de Salud y Protección Social, Colciencias, Universidad de Antioquia. Guía de práctica clínica para la prevención secundaria, diagnóstico, tratamiento y rehabilitación de la falla cardíaca en población mayor de 18 años clasificación B, C y D: Guía completa. Sistema General de Seguridad Social en Salud. Accessed on: October 1, 2018. Available at: http://gpc.minsalud.gov.co/gpc_sites/Repositorio/Conv_637/GPC_falla_cardiaca/GPC%20Falla%20Cardiaca%20Profesionales%20No%2053.pdf
Ribeiro RA, Stella SF, Camey SA, Zimerman LI, Pimentel M, Rohde LE, et al. Costeffectiveness of implantable cardioverter-defibrillators in Brazil: Primary prevention analysis in the public sector. Value Health. 2010;13:160-168. https://doi.org/10.1111/j.1524-4733.2009.00608.x
Noyes K, Veazie P, Hall WJ, Zhao H, Buttaccio A, Thevenet-Morrison K, et al. Costeffectiveness of cardiac resynchronization therapy in the MADIT-CRT trial. J Cardiovasc Electrophysiol. 2013;24:66-74. https://doi.org/10.1111/j.1540-8167.2012.02413.x
Sanders GD, Kong MH, Al-Khatib SM, Peterson ED. Cost-effectiveness of implantable cardioverter defibrillators in patients ≥65 years of age. Am Heart J. 2010;160:122-31. https://doi.org/10.1016/j.ahj.2010.04.021
Cowie MR, Marshall D, Drummond M, Ferko N, Maschio M, Ekman M, et al. Lifetime cost-effectiveness of prophylactic implantation of a cardioverter defibrillator in patients with reduced left ventricular systolic function: Results of Markov modelling in a European population. Europace. 2009;11:716-26. https://doi.org/10.1093/europace/eup068
World Health Organization. Macroeconomics and Health: Investing in health for economic development. Report for the Commission on macroeconomics and health. Accessed on: October 1, 2018. Available at: http://apps.who.int/iris/bitstream/10665/42435/1/924154550X.pdf
Smith T, Jordaens L, Theuns DA, van Dessel PF, Wilde AA, Hunink MG. The costeffectiveness of primary prophylactic implantable defibrillator therapy in patients with ischaemic or non-ischaemic heart disease: A European analysis. Eur Heart J. 2013;34:211-219. https://doi.org/10.1093/eurheartj/ehs090
Gandjour A, Holler A, Dipl-Ges-Ök, Adarkwah CC. Cost-effectiveness of implantable defibrillators after myocardial infarction based on 8-year follow-up data (MADIT II). Value Health. 2011;14:812-7. https://doi.org/10.1016/j.jval.2011.02.1180
Alcaraz A, González-Zuelgaray J, Augustovski F. Costo-efectividad del cardiodesfibrilador implantable en pacientes con factores de riesgo de muerte súbita en Argentina. Value Health. 2011;14:33-38. https://doi.org/10.1016/j.jval.2011.05.030
Epstein LM, Love CJ, Wilkoff BL, Chung MK, Hackler JW, Bongiorni MG, et al. Superior vena cava defibrillator coils make transvenous lead extraction more challenging and riskier. J Am Coll Cardiol. 2013;61:987-989. https://doi.org/10.1016/j.jacc.2012.12.014
Køber L, Thune JJ, Nielsen JC, Haarbo J, Videbæk L, Korup E, et al. Defibrillator implantation in patients with nonischemic systolic heart failure. N Engl J Med. 2016;375:1221-1230. https://doi.org/10.1056/NEJMoa1608029
Narayanan A, Reddy V, Deshmukh B, Adabag B. Efficacy of implantable cardioverter defibrillator therapy in patients with nonischemic cardiomyopathy: A systematic review and meta-analysis of randomized controlled trials. JACC Clin Electrophysiol. 2017;3:962-70. https://doi.org/10.1016/j.jacep.2017.02.006
Siddiqui WJ, Aggarwal S, Rafique M, Singh S, Kutalek S, Eisen HJ. Prophylactic use of the implantable cardioverter-defibrillator and its effect on the long-term survival, cardiovascular and sudden cardiac death in nonischemic cardiomyopathy patients-a systematic review and meta-analysis. Heart Fail Rev. 2018;23:181-90. https://doi.org/10.1007/s10741-018-9671-6
Epstein LM, Love CJ, Wilkoff BL, Chung MK, Hackler JW, Bongiorni MG, et al. Superior vena cava defibrillator coils make transvenous lead extraction more challenging and riskier. J Am Coll Cardiol. 2013;61:987-9. https://doi.org/10.1016/j.jacc.2012.12.014
Some similar items:
- Alex García, Nelson Darío Giraldo , Cost-effectiveness of extracorporeal membrane oxygenation in patients with acute respiratory distress syndrome in Colombia , Biomedica: Vol. 42 No. 4 (2022)
- Ana Helena Perea, Diego Rosselli, Immediate versus delayed breast reconstruction in breast cancer patients in Colombia: A costutility analysis , Biomedica: Vol. 38 No. 3 (2018)
- Roosevelt Fajardo, José Ignacio Valenzuela, Sandra Catalina Olaya, Gustavo Quintero, Gabriel Carrasquilla, Carlos Eduardo Pinzón, Catalina López, Juan Camilo Ramírez, Cost-effectiveness of laparoscopic versus open cholecystectomy , Biomedica: Vol. 31 No. 4 (2011)
- Óscar Gamboa, Sandra Díaz, Liliana Chicaíza, Mario García, Cost-benefit analysis of anastrazol and tamoxifen in adjuvant treatment of hormone receptor-positive, post-menopausal breast cancer , Biomedica: Vol. 30 No. 1 (2010)
- Raúl Murillo, Ricardo Cendales, Carolina Wiesner, Marion Piñeros, Sandra Tovar, Effectiveness of cytology-based cervical cancer screening in the Colombian health system , Biomedica: Vol. 29 No. 3 (2009)
- Sandra Lorena Girón, Julio César Mateus, Fabián Méndez, Impact of an open waste disposal site on the occurrence of respiratory symptoms and on health care costs of children , Biomedica: Vol. 29 No. 3 (2009)
- Luis Eduardo Echeverría, Juan Esteban Gómez-Mesa, Clara Saldarriaga, Sebastián Campbell-Quintero, Lisbeth Natalia Morales-Rodríguez, Juan David López-Ponce de León, Andrés Felipe Buitrago, Erika Martínez-Carreño, Jorge Alberto Sandoval-Luna, Alexis Llamas, Gustavo Adolfo Moreno-Silgado, Julián Vanegas-Eljach, Nelson Eduardo Murillo-Benítez, Ricardo Gómez-Palau, Alex Arnulfo Rivera-Toquica, Diabetes mellitus in patients with heart failure and effect modification of risk factors for short-term mortality: An observational study from the Colombian Heart Failure Registry (RECOLFACA) , Biomedica: Vol. 44 No. Sp. 1 (2024): Publicación anticipada, Enfermedades crónicas no transmisibles
- Andrés Páez, Gloria Rey, Carlos Agudelo, Alvaro Dulce, Edgar Parra, Hernando Díaz-Granados, Damaris Heredia, Luis Polo, Outbreak of urban rabies transmitted by dogs in Santa Marta, northern Colombia , Biomedica: Vol. 29 No. 3 (2009)
- Patricia Escobar, Katherine Paola Luna, Indira Paola Hernández, César Mauricio Rueda, María Magdalena Zorro, Simon L. Croft, In vitro susceptibility of Trypanosoma cruzi strains from Santander, Colombia, to hexadecylphosphocholine (miltefosine), nifurtimox and benznidazole , Biomedica: Vol. 29 No. 3 (2009)
- Mauricio Beltrán, María Cristina Navas, María Patricia Arbeláez, Jorge Donado, Sergio Jaramillo, Fernando De la Hoz, Cecilia Estrada, Lucía del Pilar Cortés, Amalia de Maldonado, Gloria Rey, Seroprevalence of hepatitis B virus and human immunodeficiency virus infection in a population of multiply-transfused patients in Colombia , Biomedica: Vol. 29 No. 2 (2009)
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























