Congenital Langerhans cell histiocytosis
Abstract
Langerhans cell histiocytosis is a rare pathology with different clinical manifestations in the neonatal period ranging from isolated bone lesions to systemic compromise.
We report a case of Langerhans cell histiocytosis including a literature review focused on the clinical manifestations, diagnosis, and treatment. A one-month-old patient was brought to medical consultation with lymphadenopathy and skin lesions, which were initially managed as an infectious pathology. The disease continued its progression without improvement with the treatment until the patient died due to respiratory failure.
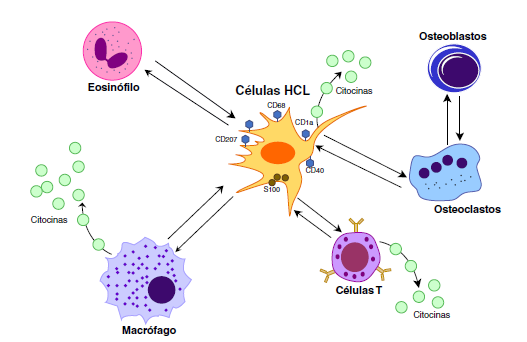
The lymph node and skin biopsies revealed infiltration of atypical cells with positive immunohistochemistry for S100, CD1, and CD68 confirming Langerhans cell histiocytosis.
This disorder represents a great challenge and, therefore, it is important to alert and sensitize medical teams about it for timely diagnosis and management.
Downloads
References
Morimoto A, Oh Y, Shioda Y, Kudo K, Imamura T. Recent advances in Langerhans cell histiocytosis. Pediatr Int. 2014;56:451-61. https://doi.org/10.1111/ped.12380
Filipovich A, McClain K, Grom A. Histiocytic disorders: Recent insights into pathophysiology and practical guidelines. Biol Blood Marrow Transplant. 2010;16(Suppl.):S82-9. https://doi.org/10.1016/j.bbmt.2009.11.014
Jaffe R. The diagnostic histopathology of Langerhans cell histiocytosis. In: Egeler RM, Weitzman S, editors. Histiocytic disorders of children and adults: Basic science, clinical features and therapy. Cambridge: Cambridge University Press; 2005. p. 14-39. https://doi.org/10.1017/CBO9780511545252.003
Jezierska M, Stefanowicz J, Romanowicz G, Kosiak W, Lange M. Langerhans cell histiocytosis in children - a disease with many faces. Recent advances in pathogenesis, diagnostic examinations and treatment. Postepy Dermatol Alergol. 2018;35:6-17. https://doi.org/10.5114/pdia.2017.67095
Abla O, Egeler RM, Weitzman S. Langerhans cell histiocytosis: Current concepts and treatments. Cancer Treat Rev. 2010;36:354-9. https://doi.org/10.1016/j.ctrv.2010.02.012
Grana N. Langerhans cell histiocytosis. Cancer Control. 2014;21:328-34. https://doi.org/10.1177/107327481402100409
Salotti JA, Nanduri V, Pearce MS, Parker L, Lynn R, Windebank KP. Incidence and clinical features of Langerhans cell histiocytosis in the UK and Ireland. Arch Dis Child. 2009;94:376-80. https://doi.org/10.1136/adc.2008.144527
Castro EC, Blázquez C, Boyd J, Correa H, de Chadarevian JP, Felgar RE, et al. Clinicopathologic features of histiocytic lesions following ALL, with a review of the literature. Pediatr Dev Pathol. 2010;13:225-37. https://doi.org/10.2350/09-03-0622-OA.1
Krooks J, Minkov M, Weatherall AG. Langerhans cell histiocytosis in children: Diagnosis, differential diagnosis, treatment, sequelae, and standardized follow-up. J Am Acad Dermatol. 2018;78:1047-56. https://doi.org/10.1016/j.jaad.2017.05.060
Frade AP, Godinho MM, Batalha AB, Bueno APS. Congenital Langerhans cell histiocytosis: A good prognosis disease? An Bras Dermatol. 2017;92:40-2. https://doi.org/10.1590/abd1806-4841.20175308
Grois N, Pötschger U, Prosch H, Minkov M, Arico M, Braier J, et al. Risk factors for diabetes insipidus in langerhans cell histiocytosis. Pediatr Blood Cancer. 2006;46:228-33. https://doi.org/10.1002/pbc.20425
Merglova V, Hrusak D, Boudova L, Mukensnabl P, Valentova E, Hosticka L. Langerhans cell histiocytosis in childhood - review, symptoms in the oral cavity, differential diagnosis and report of two cases. J Craniomaxillofac Surg. 2014;42:93-100. https://doi.org/10.1016/j.jcms.2013.03.005
Krooks J, Minkov M, Weatherall AG. Langerhans cell histiocytosis in children: History, classification, pathobiology, clinical manifestations, and prognosis. J Am Acad Dermatol. 2018;78:1035-44. https://doi.org/10.1016/j.jaad.2017.05.059
Kapur P, Erickson C, Rakheja D, Carder KR, Hoang MP. Congenital self-healing reticulohistiocytosis (Hashimoto-Pritzker disease): Ten-year experience at Dallas Children’s Medical Center. J Am Acad Dermatol. 2007;56:290-4. https://doi.org/10.1016/j.jaad.2006.09.001
Berres ML, Merad M, Allen CE. Progress in understanding the pathogenesis of Langerhans cell histiocytosis: Back to histiocytosis X? Br J Haematol. 2015;169:3-13. https://doi.org/10.1111/bjh.13247
Gadner H, Heitger A, Grois N, Gatterer-Menz I, Ladisch S. Treatment strategy for disseminated langerhans cell histiocytosis. Med Pediatr Oncol. 1994;23:72-80. https://doi.org/10.1002/mpo.2950230203
Hutter C, Minkov M. Insights into the pathogenesis of Langerhans cell histiocytosis: The development of targeted therapies. Immunotargets Ther. 2016;5:81-91. https://doi.org/10.2147/ITT.S91058
Nakajima K, Morisawa R, Kodama H, Sano S. Successful treatment with cyclophosphamide of Langerhans cell histiocytosis involving the skin and lymph nodes in an adult patient. Clin Exp Dermatol. 2010;35:791-2. https://doi.org/10.1111/j.1365-2230.2010.03802.x
Gadner H, Grois N, Arico M, Broadbent V, Ceci A, Jakobson A, et al. A randomized trial of treatment for multisystem Langerhans cell histiocytosis. J Pediatr. 2001;138:728-34. https://doi.org/10.1067/mpd.2001.111331
Morimoto A, Ikushima S, Kinugawa N, Ishii E, Kohdera U, Sako M, et al. Improved outcome in the treatment of pediatric multifocal Langerhans cell histiocytosis. Cancer. 2006;107:613-9. https://doi.org/10.1002/cncr.21985
Ronceray L, Pötschger U, Janka G, Gadner H, Minkov M. Pulmonary involvement in pediatric-onset multisystem langerhans cell histiocytosis: Effect on course and outcome. J Pediatr. 2012;161:129-33.e3. https://doi.org/10.1016/j.jpeds.2011.12.035
Gadner H, Minkov M, Grois N, Pötschger U, Thiem E, Aricò M, et al. Therapy prolongation improves outcome in multisystem Langerhans cell histiocytosis. Blood. 2013;121:5006-14. https://doi.org/10.1182/blood-2012-09-455774
Some similar items:
- Lorena Peñaloza, Catalina Forero, Camila Céspedes, Characterization of patients diagnosed with congenital hypothyroidism at the Hospital Universitario San Ignacio between 2001 and 2017 , Biomedica: Vol. 40 No. 3 (2020)
- Jaime E. Bernal, Martha Lucía Tamayo , Ignacio Briceño , Escilda Benavides , Newborn screening in Colombia: The experience of a private program in Bogotá , Biomedica: Vol. 44 No. 1 (2024)
- Beatriz Eugenia Alvarado, Luis Reinel Vásquez, Social determinants, feeding practices and nutritional consequences of intestinal parasitism in young children. , Biomedica: Vol. 26 No. 1 (2006)
- Jairo Echeverry, Carlos Mauricio Hurtado, Myriam Gutiérrez, Clinical manifestations of lead levels in children exposed to automobile battery recycling processes in Soacha and Bogotá, D.C. , Biomedica: Vol. 28 No. 1 (2008)
- Juan Gabriel Piñeros, Margarita Arboleda, Juan Camilo Jaramillo, Silvia Blair, Report of five cases of severe neonatal Plasmodium vivax malaria in Urabá, Colombia , Biomedica: Vol. 28 No. 4 (2008)
- Raúl Murillo, Ricardo Cendales, Carolina Wiesner, Marion Piñeros, Sandra Tovar, Effectiveness of cytology-based cervical cancer screening in the Colombian health system , Biomedica: Vol. 29 No. 3 (2009)
- Sandra Lorena Girón, Julio César Mateus, Fabián Méndez, Impact of an open waste disposal site on the occurrence of respiratory symptoms and on health care costs of children , Biomedica: Vol. 29 No. 3 (2009)
- Andrés Páez, Gloria Rey, Carlos Agudelo, Alvaro Dulce, Edgar Parra, Hernando Díaz-Granados, Damaris Heredia, Luis Polo, Outbreak of urban rabies transmitted by dogs in Santa Marta, northern Colombia , Biomedica: Vol. 29 No. 3 (2009)
- Patricia Escobar, Katherine Paola Luna, Indira Paola Hernández, César Mauricio Rueda, María Magdalena Zorro, Simon L. Croft, In vitro susceptibility of Trypanosoma cruzi strains from Santander, Colombia, to hexadecylphosphocholine (miltefosine), nifurtimox and benznidazole , Biomedica: Vol. 29 No. 3 (2009)
- Mauricio Beltrán, María Cristina Navas, María Patricia Arbeláez, Jorge Donado, Sergio Jaramillo, Fernando De la Hoz, Cecilia Estrada, Lucía del Pilar Cortés, Amalia de Maldonado, Gloria Rey, Seroprevalence of hepatitis B virus and human immunodeficiency virus infection in a population of multiply-transfused patients in Colombia , Biomedica: Vol. 29 No. 2 (2009)
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























