Direct costs of neonatal infection acquired in the community in full-term newborns and low risk at birth, Cundinamarca, Colombia
Abstract
Introduction: Half of the episodes of neonatal sepsis are acquired in the community with a high percentage of mortality and complications.
Objective: To estimate the direct costs of hospitalizations due to systemic neonatal infection acquired in the community in low-risk newborns.
Materials and methods: For the estimation of costs, we used the perspective of the health systems and the microcosting technique and we established the duration of hospitalization as the time horizon. We identified cost-generating events through expert consensus and the quantification was based on the detailed bill of 337 hospitalized newborns diagnosed with neonatal infection. The costs of the medications were calculated based on the drug price information system (SISMED) and the ISS 2001 rate manuals adjusting percentage, and the mandatory insurance rates for traffic accidents (SOAT). We used the bootstrapping method for cost distribution to incorporate data variability in the estimate.
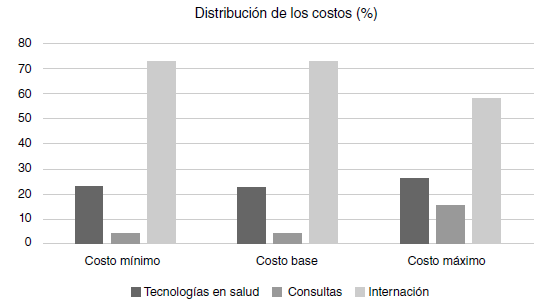
Results: We included the medical care invoices for 337 newborns. The average direct cost of care per patient was USD$ 2,773,965 (Standard Deviation, SD=USD$ 198,813.5; 95% CI: $ 2,384,298 - $ 3,163,632). The main cost-generating categories were hospitalization in intensive care units and health technologies. The costs followed a log-normal distribution.
Conclusions: The categories generating the greatest impact on the care costs of newborns with infection were hospitalization in neonatal units and health technologies. The costs followed a log-normal distribution.
Downloads
References
Yang X, Meng T. Admission of full-term infants to the neonatal intensive care unit: A 9.5-year review in a tertiary teaching hospital. J Matern Neonatal Med. 2020;33:3003-9. https://doi.org/10.1080/14767058.2019.1566901
Santos Burgoa-Larrañaga L, Iglesias-Leboreiro J, Bernardez-Zapata I. Early discharge of the healthy newborn from the nursery of the Hospital Español de México. Rev Med Inst Mex Seguro Soc. 2016;54:696-705.
Harron K, Gilbert R, Cromwell D, Oddie S, van der Meulen J. Newborn length of stay and risk of readmission. Paediatr Perinat Epidemiol. 2017;31:221-32. https://doi.org/10.1111/ppe.12359
Waters D, Jawad I, Ahmad A, Lukšić I, Nair H, Zgaga L, et al. Aetiology of communityacquired neonatal sepsis in low- and middle-income countries. J Glob Health. 2011;1:154-70.
Weber MW, Carlin JB, Gatchalian S, Lehmann D, Muhe L, Mulholland EK. Predictors of neonatal sepsis in developing countries. Pediatr Infect Dis J. 2003;22:711-7. https://doi.org/10.1097/01.inf.0000078163.80807.88
Osrin D, Vergnano S, Costello A. Serious bacterial infections in newborn infants in developing countries. Curr Opin Infect Dis. 2004;17:217-24. https://doi.org/10.1097/00001432-200406000-00008
Downie L, Armiento R, Subhi R, Kelly J, Clifford V, Duke T. Community-acquired neonatal and infant sepsis in developing countries: Efficacy of WHO’s currently recommended antibiotics -Systematic review and meta-analysis. Arch Dis Child. 2013;98:146-54. https://doi.org/10.1136/archdischild-2012-30203
Jaramillo-Mejía MC, Chernichovsky D, Jiménez-Moleón JJ. Brechas regionales de la mortalidad infantil en Colombia. Rev Peru Med Exp Salud Pública. 2014;30:550-9.
Stoll BJ, Gary L. Darmstadt AK. Neonatal infections: A global perspective. En: Wilson C, Nizet V, Maldonado Y, Remington J. Klein J, editors. Remington and Klein’s Infectious diseases of the fetus and newborn infant. Eighth edition. Amsterdam: Saunders; 2016. p. 24-53.
Bulkowstein S, Ben-Shimol S, Givon-Lavi N, Melamed R, Shany E, Greenberg D. Comparison of early onset sepsis and community-acquired late onset sepsis in infants less than 3 months of age. BMC Pediatr. 2016;16:82. https://doi.org/10.1186/s12887-016-0618-6
Lantos JD, Meadow WL. Costs and end-of-life care in the NICU: Lessons for the MICU? J Law, Med Ethics. 2011;39:194-200. https://doi.org/10.1111/j.1748-720X.2011.00588.x
Mugford M. Outcome and cost of neonatal intensive care. Curr Paediatr. 1994;4:30-2.
WHO. Disease burden and mortality estimates. Geneva: WHO; 2019. Fecha de consulta: 6 de agosto de 2020. Disponible en: http://www.who.int/healthinfo/global_burden_disease/estimates/en/
Murthy S, John D, Godinho IP, Godinho MA, Guddattu V, Nair NS. A protocol for a systematic review of economic evaluation studies conducted on neonatal systemic infections in South Asia. Syst Rev. 2017;6:252. https://doi.org/10.1186/s13643-017-0648-7
Mejía-Mejía A, Moreno-Viscaya M. Evaluación económica para la toma de decisiones en salud en Colombia. Superintendencia Nacional de Salud. 2014;5:70-7.
Departamento Administrativo Nacional de Estadísticas, DANE. Defunciones no fetales. Internet. Primeras causas de defunción. 2019. Fecha de consulta: 6 de agosto de 2020. Disponible en: https://www.dane.gov.co/index.php/estadisticas-por-tema/salud/nacimientosy-defunciones/defunciones-no-fetales
Liu L, Oza S, Hogan D, Chu Y, Perin J, Zhu J, et al. Global, regional, and national causes of under-5 mortality in 2000–15: An updated systematic analysis with implications for the Sustainable Development Goals. Lancet. 2016;388:3027-35. https://doi.org/10.1016/S0140-6736(16)31593-8
Cheah IGS. Economic assessment of neonatal intensive care. Transl Pediatr. 2019;8:246-56. https://doi.org/10.21037/tp.2019.07.03
Alvarado-Jaramillo JC, Gonzáles-Ramos AJ, Mendoza-Arana P. Análisis de costos en dos unidades de cuidados intensivos pediátricos del Ministerio de Salud del Perú. Anales de la Facultad de Medicina. 2011;72:249-54.
Shanmugasundaram R, Padmapriya E, Shyamala J. Cost of neonatal intensive care. Indian J Pediatr. 1998;65:249-55. https://doi.org/10.1007/BF02752301
Profit J, Lee D, Zupancic JA, Papile L, Gutiérrez C, Goldie SJ, et al. Clinical benefits, costs, and cost-effectiveness of neonatal intensive care in México. PLoS Med. 2010;7:e1000379. https://doi.org/10.1371/journal.pmed.1000379
Amador-Morán R, Labrada-Despaigne A, Campo-González A, Díaz-Aguilar R. Costo-beneficio en una unidad de cuidados intensivos neonatales. Rev Cubana Pediatr. 2011;83:166-72.
Lassi ZS, Bhutta ZA. Community-based intervention packages for reducing maternal and neonatal morbidity and mortality and improving neonatal outcomes. Cochrane Database Syst Rev. 2015;3:CD007754. https://doi.org/10.1002/14651858.CD007754.pub3
Nkonki LL, Chola LL, Tugendhaft AA, Hofman KK. Modelling the cost of community interventions to reduce child mortality in South Africa using the Lives Saved Tool (LiST). BMJ Open. 2017;7:e011425. https://doi.org/10.1136/bmjopen-2016-011425
Mangham-Jefferies L, Pitt C, Cousens S, Mills A, Schellenberg J. Cost-effectiveness of strategies to improve the utilization and provision of maternal and newborn health care in low-income and lower-middle-income countries: A systematic review. BMC Pregnancy Childbirth. 2014;14:243. https://doi.org/10.1186/1471-2393-14-243
Bhutta ZA, Das JK, Bahl R, Lawn JE, Salam RA, Paul VK, et al. Can available interventions end preventable deaths in mothers, newborn babies, and stillbirths, and at what cost? Lancet. 2014;384:347-70. https://doi.org/10.1016/S0140-6736(14)60792-3
Ranjeva SL, Warf BC, Schiff SJ. Economic burden of neonatal sepsis in sub-Saharan Africa. BMJ Glob Health. 2018;3:e000347. https://doi.org/10.1136/bmjgh-2017-000347
Some similar items:
- Hernando Baquero, María Elena Venegas Martinez, Lorena Velandia Forero, Fredy Neira Safi, Edgar Navarro, Neonatal late-onset infection with SARS CoV-2 , Biomedica: Vol. 40 No. Supl. 2 (2020): SARS-CoV-2 y COVID-19
- Gerardo Quintana, Claudia Mora, Andrés González, Jorge Díaz Díaz, Financial cost of early rheumatoid arthritis in the first year medical attention: three clinical scenarios. , Biomedica: Vol. 29 No. 1 (2009)
- Albenia Lurán, Elizabeth López, Consuelo Pinilla, Pedro Sierra, Mortality by avoidable causes in preschool children , Biomedica: Vol. 29 No. 1 (2009)
- Ignacio Zarante, Liliana Franco, Catalina López, Nicolás Fernández, Frequencies of congenital malformations: assessment and prognosis of 52,744 births in three cities of Colombia , Biomedica: Vol. 30 No. 1 (2010)
- José Fernando Pinzón, Carlos Maldonado, Jorge A. Díaz, Omar Segura, Direct costs and hospital morbimortality impact from preventable adverse drug events , Biomedica: Vol. 31 No. 3 (2011)
- Edwin Fernando Quiroga, Death rate by malnutrition in children under the age of five, Colombia , Biomedica: Vol. 32 No. 4 (2012)
- Martín Romero, Diana Chávez, Magalí De los Ríos, Nelson Alvis-Guzmán, Cost-effectiveness of nilotinib, dasatinib and imatinib as first-line treatment for chronic myeloid leukemia in Colombia, 2012 , Biomedica: Vol. 34 No. 1 (2014)
- Liliana I. Barrero, Juan S. Castillo, Aura L. Leal, Ricardo Sánchez, Jorge A. Cortés, Carlos A. Álvarez, Andrés L. González, Economic burden of methicillin-resistant Staphylococcus aureus bacteremia in critical care patients in hospitals in Bogotá , Biomedica: Vol. 34 No. 3 (2014)
- Cristian Vallejo, Yolanda Cifuentes, Characterization and six-month follow-up on a cohort of newborns with congenital syphilis , Biomedica: Vol. 36 No. 1 (2016)
- Mary A. García, Luisa Imbachí, Paula M. Hurtado, Gloria Gracia, Ignacio Zarante, Ultrasound detection of congenital anomalies in 76,155 births in the cities of Bogotá and Cali, 2011-2012 , Biomedica: Vol. 34 No. 3 (2014)
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























