Expression of the inflammasome components and its relationship with cardiovascular risk markers in people living with HIV-1
Abstract
Introduction: HIV-1 infection induces a chronic inflammatory state in which inflammasomes participate. The increase in inflammatory parameters is higher in individuals with active viral replication (progressors) than in those with viral control (HIV-1 controllers). This process triggers metabolic alterations related to changes in the lipid profile, which could increase the risk of cardiovascular events, even in patients with antiretroviral therapy.
Objective: To establish whether there was a correlation between the expression of inflammasome components and cardiovascular risk markers in HIV-1 controllers and progressors with or without antiretroviral therapy.
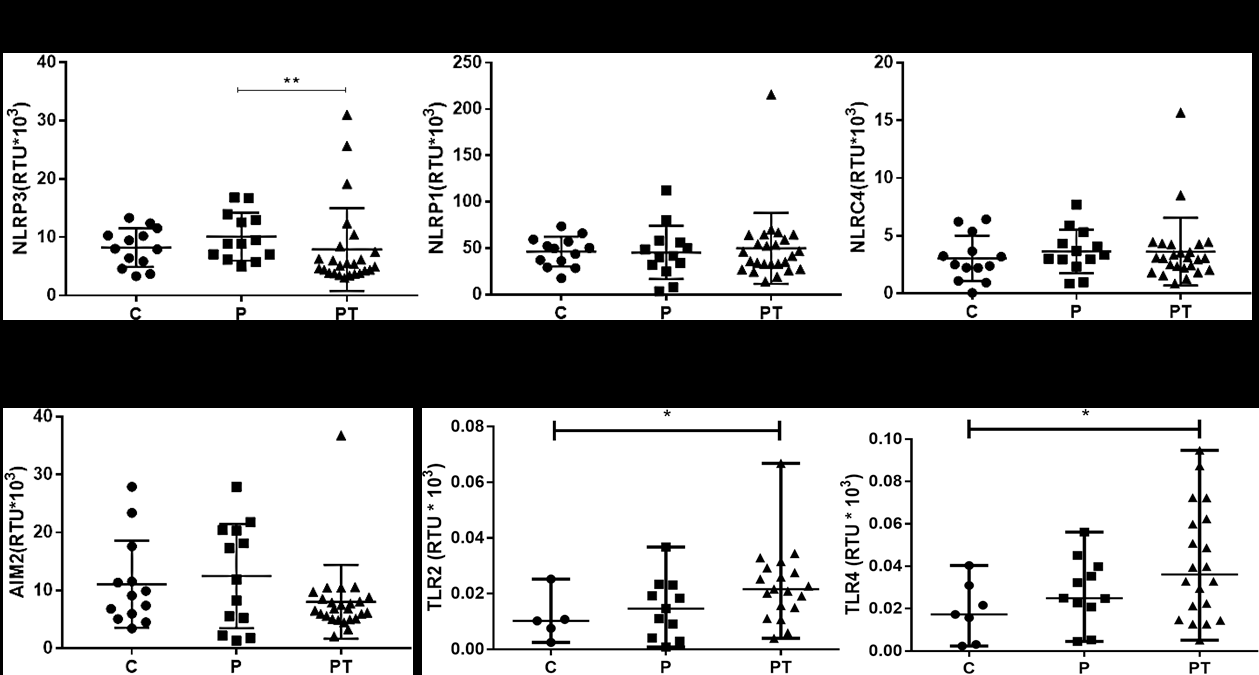
Materials and methods: We studied 13 HIV-1 controllers and 40 progressors (19 without antiretroviral therapy and 31 with therapy) and evaluated in them classic markers of cardiovascular risk. Using RT-PCR we quantified the expression of inflammasome components (NLRP1, NLRP3, NLRC4, AIM2, ASC, IL-1β, IL-18, and caspase-1), TLR2, TLR4, TGF-β, and IL-10.
Results: Progressors with antiretroviral therapy had an increased expression of TLR2, TLR4, and IL-18 compared to HIV-1 controllers. They also showed high levels of triglycerides and VLDL, which positively correlated with the expression of the inflammasome components NLRP1, NLRP3, NLRC4, AIM2, ASC, and caspase-1.
Conclusion: Progressors receiving antiretroviral therapy exhibited an increased expression of the inflammasome components, which correlated with the levels of triglycerides and VLDL. This supports the role of inflammation in cardiovascular risk during HIV-1 infection.
Downloads
References
Walker BD. Elite control of HIV Infection: Implications for vaccines and treatment. Top HIV Med. 2007;15:134-6.
Gonzalo-Gil E, Ikediobi U, Sutton RE. Mechanisms of virologic control and clinical characteristics of HIV+ elite/viremic controllers. Yale J Biol Med. 2017;90:245-59.
Deeks S, Tracy R, Douek D. Systemic effects of inflammation on health during chronic HIV infection. Immunity. 2013;39:633-45. https://doi.org/10.1016/j.immuni.2013.10.001.Systemic
Deeks S. Immune dysfunction, inflammation, and accelerated aging in patients on antiretroviral therapy. Top HIV Med. 2009;14:118-23
Lucas S, Nelson AM. HIV and the spectrum of human disease. J Pathol. 2015;235:229-41. https://doi.org/10.1002/path.4449
Kedzierska K, Crowe SM. Cytokines and HIV-1: Interactions and clinical implications. Antivir Chem Chemother. 2001;12:133-50. https://doi.org/10.1177/095632020101200301
Ahmad R, Sindhu STA, Toma E, Morisset R, Ahmad A. Elevated levels of circulating interleukin-18 in human immunodeficiency virus-infected individuals: Role of peripheral blood mononuclear cells and implications for AIDS pathogenesis. J Virol. 2002;76:12448-56. https://doi.org/10.1128/jvi.76.24.12448-12456.2002
Granowitz E V, Saget BM, Wang MZ, Dinarello CA, Skolnik PR. Interleukin 1 induces HIV-1 expression in chronically infected U1 cells: Blockade by interleukin 1 receptor antagonist and tumor necrosis factor binding protein type 1. Mol Med. 1995;1:667-77. https://doi.org/10.1007/bf03401607
Shapiro L, Puren AJ, Barton HA, Novick D, Peskind RL, Shenkar R, et al. Interleukin 18 stimulates HIV type 1 in monocytic cells. Proc Natl Acad Sci U S A. 1998;95:12550-5. https://doi.org/10.1073/pnas.95.21.12550
Swingler S, Easton A, Morris A. Cytokine augmentation of HIV-1 LTR-driven gene expression in neural cells. AIDS Res Hum Retroviruses. 1992;8:487-93. https://doi.org/10.1089/aid.1992.8.487
Martínez GJ, Celermajer DS, Patel S. The NLRP3 inflammasome and the emerging role of colchicine to inhibit atherosclerosis-associated inflammation. Atherosclerosis. 2018;269:262-71. https://doi.org/10.1016/j.atherosclerosis.2017.12.027
Mullis C, Swartz TH. NLRP3 Inflammasome signaling as a link between HIV-1 infection and atherosclerotic cardiovascular disease. Front Cardiovasc Med. 2020;7:1-11. https://doi.org/10.3389/fcvm.2020.00095
Yazdi AS, Ghoreschi K. The interleukin-1 family. Adv Exp Med Biol. 2016;941:21-9. https://doi.org/10.1007/978-94-024-0921-5
Broz P, Monack DM. Newly described pattern recognition receptors team up against intracellular pathogens. Nat Rev Immunol. 2013;13:551-65. https://doi.org/10.1038/nri3479
Hernández JC, Latz E, Urcuqui-Inchima S. HIV-1 induces the first signal to activate the NLRP3 inflammasome in monocyte-derived macrophages. Intervirology. 2014;57:36-42. https://doi.org/10.1159/000353902
Feria MG, Taborda NA, Hernández JC, Rugeles MT. HIV replication is associated to inflammasomes activation, IL-1β, IL-18 and caspase-1 expression in GALT and peripheral blood. PLoS One. 2018;13:1-14. https://doi.org/10.1371/journal.pone.0192845
Ahmad F, Mishra N, Ahrenstorf G, Franklin BS, Latz E, Schmidt RE, et al. Evidence of inflammasome activation and formation of monocyte-derived ASC specks in HIV-1 positive patients. AIDS. 2018;32:299-307. https://doi.org/10.1097/QAD.0000000000001693
Bociaga-Jasik M, Polus A, Góralska J, Śliwa A, Raź́ny U, Zdzienicka A, et al. Metabolic complications and selected cytokines in HIV-infected individuals. Pol Arch Med Wewn. 2014;124:27-35. https://doi.org/10.20452/pamw.2073
Umeh OC, Currier JS. Lipids, metabolic syndrome, and risk factors for future cardiovascular disease among HIV-infected patients. Curr HIV/AIDS Rep. 2005;2:132-9. https://doi.org/10.1007/s11904-005-0006-6
Tall AR, Yvan-Charvet L. Cholesterol, inflammation and innate immunity. Nat Rev Immunol. 2015;15:104-16. https://doi.org/10.1038/nri3793
Arias-Pérez R, Álvarez N, Sánchez-Gómez C, Flórez-Álvarez L, Marín-Palma D, Taborda NA, et al. Alteración en la expresión de proteínas transportadoras de colesterol y moléculas inmunomoduladoras en pacientes con VIH-1. Kasmera. 2021;49:1-13. https://doi.org/10.5281/zenodo.4780969
Hoseini Z, Sepahvand F, Rashidi B, Sahebkar A, Masoudifar A, Mirzaei H. NLRP3 inflammasome: Its regulation and involvement in atherosclerosis. J Cell Physiol. 2018;233:2116-32. https://doi.org/10.1002/jcp.25930
Tabares-Guevara J, Villa-Pulgarín J, Hernández JC. Atherosclerosis: Immunopathogenesis and strategies for immunotherapy. Immunotherpay. 2021;13:1. https://doi.org/10.2217/imt-2021-0009
Raposeiras-Roubín S, Triant V. Ischemic heart disease in HIV: An in-depth look at cardiovascular risk. Rev Española Cardiol. 2016;69:1204-13. https://doi.org/10.1016/j.rec.2016.10.005
Zicari S, Sessa L, Cotugno N, Ruggiero A, Morrocchi E, Concato C, et al. Immune activation, inflammation, and non-AIDS co-morbidities in HIV-infected patients under long-term ART. Viruses. 2019;11:1-19. https://doi.org/10.3390/v11030200
Marín-Palma D, Castro GA, Cardona-Arias JA, Urcuqui-Inchima S, Hernández JC. Lower high-density lipoproteins levels during human immunodeficiency virus type 1 infection are associated with increased inflammatory markers and disease progression. Front Immunol. 2018;9:1-12. https://doi.org/10.3389/fimmu.2018.01350
Marín-Palma D, Cardona-Arias JA, Hernández JC. Factores inmunológicos relacionados con VIH-1 en pacientes colombianos. Revista Ciencias de la Salud. 2019;17:245-58. https://doi.org/10.12804/revistas.urosario.edu.co/revsalud/a.7927
Schneider E, Whitmore S, Glynn KM, Domínguez K, Mitsch A, McKenna MT. et al. Revised surveillance case definitions for HIV infection among adults, adolescents, and children aged <18 months and for HIV infection and AIDS among children aged 18 months to <13 years —United States. MMWR Recomm Rep. 2008;57:1-12.
Khera AV, Cuchel M, de la Llera-Moya M, Rodrigues A, Burke MF, Jafri K, et al. Cholesterol efflux capacity, high-density lipoprotein function, and atherosclerosis. N Engl J Med. 2011;364:127-35. https://doi.org/10.1056/nejmoa1001689
Thomas MR, Lip GYH. Novel risk markers and risk assessments for cardiovascular disease. Circ Res. 2017;120:133-49. https://doi.org/10.1161/CIRCRESAHA.116.309955
Yvan-Charvet L, Bonacina F, Guinamard RR, Norata GD. Immunometabolic function of cholesterol in cardiovascular disease and beyond. Cardiovasc Res. 2019;115:1393-407. https://doi.org/10.1093/cvr/cvz127
Golia E, Limongelli G, Natale F, Fimiani F, Maddaloni V, Pariggiano I, et al. Inflammation and cardiovascular disease: From pathogenesis to therapeutic target. Curr Atheroscler Rep. 2014;16:1-7. https://doi.org/10.1007/s11883-014-0435-z
Bandera A, Masetti M, Fabbiani M, Biasin M, Muscatello A, Squillace N, et al. The NLRP3 inflammasome is upregulated in HIV-infected antiretroviral therapy-treated individuals with defective immune recovery. Front Immunol. 2018;9:1-8. https://doi.org/10.3389/fimmu.2018.00214
Toksoy A, Sennefelder H, Adam C, Hofmann S, Trautmann A, Goebeler M, et al. Potent NLRP3 inflammasome activation by the HIV reverse transcriptase inhibitor abacavir. J Biol Chem. 2017;292:2805-14. https://doi.org/10.1074/jbc.M116.749473
Luo H, He J, Qin L, Chen Y, Chen L, Li R, et al. Mycoplasma pneumoniae lipids license TLR-4 for activation of NLRP3 inflammasome and autophagy to evoke a proinflammatory response. Clin Exp Immunol. 2020;203:66-79. https://doi.org/10.1111/cei.13510
Taborda NA, Blanquiceth Y, Urcuqui-Inchima S, Latz E, Hernández JC. High-density lipoproteins decrease proinflammatory activity and modulate the innate immune response. J Interf Cytokine Res. 2019;39:760-70. https://doi.org/10.1089/jir.2019.0029
Libby P. Interleukin-1 beta as a target for atherosclerosis therapy: Biological basis of CANTOS and beyond. J Am Coll Cardiol. 2017;70:2278-89. https://doi.org/10.1016/j.jacc.2017.09.028
Rocha DM, Caldas AP, Oliveira LL, Bressan J, Hermsdorff HH. Saturated fatty acids trigger TLR4-mediated inflammatory response. Atherosclerosis. 2016;244:211-5. https://doi.org/10.1016/j.atherosclerosis.2015.11.015
Hocini H, Bonnabau H, Lacabaratz C, Lefebvre C, Tisserand P, Foucat E, et al. HIV controllers have low inflammation associated with a strong HIV-specific immune response in blood. J Virol. 2019;93:1-14. https://doi.org/10.1128/jvi.01690-18
Hileman CO, Funderburg NT. Inflammation, immune activation, and antiretroviral therapy in HIV. Curr HIV/AIDS Rep. 2017;14:93-100. https://doi.org/10.1007/s11904-017-0356-x
Hsue PY, Waters DD. HIV infection and coronary heart disease: Mechanisms and management. Nat Rev Cardiol. 2019;16:745-59. https://doi.org/10.1038/s41569-019-0219-9
Feinstein MJ, Hsue PY, Benjamin LA, Bloomfield GS, Currier JS, Freiberg MS, et al. Characteristics, prevention, and management of cardiovascular disease in people living with HIV: A scientific statement from the American Heart Association. Circulation. 2019;140:e98-124. https://doi.org/10.1161/CIR.0000000000000695
Hsue PY, Waters DD. Time to recognize HIV infection as a major cardiovascular risk factor. Circulation. 2018;138:1113-5. https://doi.org/10.1161/CIRCULATIONAHA.118.036211
Osuji FN, Onyenekwe CC, Ahaneku JE, Ukibe NR. The effects of highly active antiretroviral therapy on the serum levels of pro-inflammatory and anti-inflammatory cytokines in HIV infected subjects. J Biomed Sci. 2018;25:1-8. https://doi.org/10.1186/s12929-018-0490-9
Theron AJ, Anderson R, Rossouw TM, Steel HC. The role of transforming growth factor beta-1 in the progression of HIV/AIDS and development of Non-AIDS-defining fibrotic disorders. Front Immunol. 2017;8:1-15. https://doi.org/10.3389/fimmu.2017.01461
Orsilles MÁ, Pieri E, Cooke P, Caula C. IL-2 and IL-10 serum levels in HIV-1-infected patients with or without active antiretroviral therapy. Apmis. 2006;114:55-60. https://doi.org/10.1111/j.1600-0463.2006.apm_108.x
Girndt M, Köhler H. Interleukin-10 (IL-10): An update on its relevance for cardiovascular risk. Nephrol Dial Transplant. 2003;18:1976-9. https://doi.org/10.1093/ndt/gfg311
Lu S, Zhong J, Huang K, Zhou H. Association of IL-10-1082A/G polymorphism with cardiovascular disease risk: Evidence from a case–control study to an updated metaanalysis. Mol Genet Genomic Med. 2019;7:1-11. https://doi.org/10.1002/mgg3.888
Yilmaz MI, Solak Y, Saglam M, Cayci T, Acikel C, Unal HU, et al. The relationship between IL-10 levels and cardiovascular events in patients with CKD. Clin J Am Soc Nephrol. 2014;9:1207-16. https://doi.org/10.2215/CJN.08660813
Kaplan RC, Landay AL, Hodis HN, Gange SJ, Norris PJ, Young M, et al. Potential cardiovascular disease risk markers among HIV-infected women initiating antiretroviral treatment. J Acquir Immune Defic Syndr. 2012;60:359-68. https://doi.org/10.1097/QAI.0b013e31825b03be
Masenga S, Elijovich F, Koethe J, Hamooya B, Heimburger D, Munsaka S, et al. Hypertension and metabolic syndrome in HIV-infected patients. Curr Hypertens Rep. 2020;22:1-8. https://doi.org/https://doi.org/10.1007/s1190-020-01089-3
Ji S, Xu Y, Han D, Peng X, Lu X, Brockmeyer NH, et al. Changes in lipid indices in HIV+ cases on HAART. Biomed Res Int. 2019;2019:1-8. https://doi.org/10.1155/2019/2870647
Castro G, León K, Marín-Palma D, Oyuela S, Cataño-Bedoya JU, Duque-Botero J, et al. Evaluation of differences in metabolic and immunologic markers and cardiovascular risk in HIV-1 patients. Revista Ciencias de la Salud. 2021;19:1-18. https://doi.org/https://doi.org/10.12804/revistas.urosario.edu.co/revsalud/a
Some similar items:
- Carlos Julio Montoya, Zoraída Ramirez, Juan Carlos Cataño, Alejandro Román, María Teresa Rugeles, Effect of opportunistic infections on the frequency of leukocyte subpopulations from type-1 human immunodeficiency virus infected individuals , Biomedica: Vol. 28 No. 1 (2008)
- Juan Carlos Hernández, Carlos Julio Montoya, Silvio Urcuqui-Inchima, The role of toll-like receptors in viral infections: HIV-1 as a model , Biomedica: Vol. 27 No. 2 (2007)
- Wbeimar Aguilar-Jiménez, Wildeman Zapata, María Teresa Rugeles, Differential expression of human beta defensins in placenta and detection of allelic variants in the DEFB1 gene from HIV-1 positive mothers , Biomedica: Vol. 31 No. 1 (2011)
- Jorge Boshell, Carlos Alvarez, Sonia Marrugo, María Consuelo Rojas, Blanca Marina Rodríguez, Martha González, Berta Gómez, Immunofluorescent antibody test as additional confirmation of HIV-1infection: seven years of use at the Colombia National Institute of Health , Biomedica: Vol. 22 No. 1 (2002)
- Jorge Alejandro Henao, Nora Vanegas, Oscar David Cano, Juan Carlos Hiromi, María Teresa Rugeles, The human immunodeficiency virus type 1 and the developing central nervous system. , Biomedica: Vol. 25 No. 1 (2005)
- Jorge A. Vega, Simón Villegas-Ospina, Wbeimar Aguilar-Jiménez, María T. Rugeles, Gabriel Bedoya, Wildeman Zapata, Haplotypes in CCR5-CCR2, CCL3 and CCL5 are associated with natural resistance to HIV-1 infection in a Colombian cohort , Biomedica: Vol. 37 No. 2 (2017)
- Julio Cesar Martínez, Factors associated to mortality by non-communicable diseases in Colombia, 2008-2012 , Biomedica: Vol. 36 No. 4 (2016)
- Alejandra Moreno, Lola Xiomara Bautista, Fabio Martínez , Cardiac disease discrimination from 3D-convolutional kinematic patterns on cine-MRI sequences , Biomedica: Vol. 44 No. Sp. 1 (2024): Enfermedades crónicas no transmisibles
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























