Profile of gastrointestinal diseases in a pediatric gastroenterology center in Colombia: 15 years of follow-up
Abstract
Introduction: The profile of gastrointestinal diseases is constantly changing globally and locally affecting suspected diagnosis and medical methods.
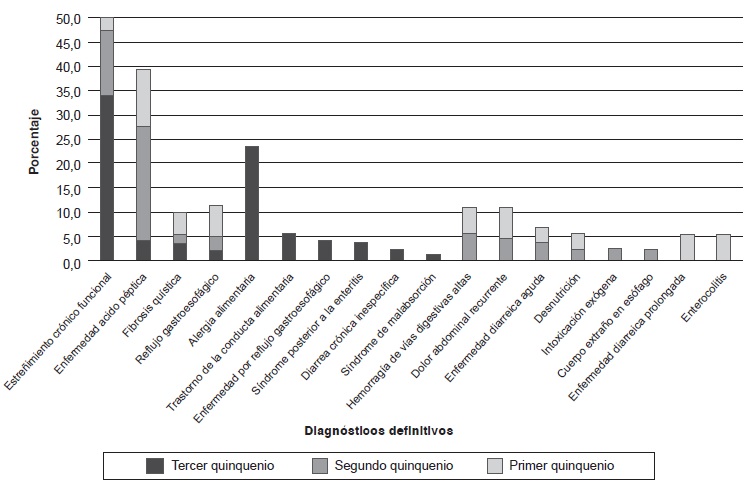
Objective: To establish the main diagnoses in a gastroenterology, hepatology, and pediatric nutrition unit in Bogota between 2009 and 2013, and to compare with findings from the same unit during the two prior five-year periods (1997 to 2006).
Materials and methods: We conducted a retrospective descriptive study. Medical records were reviewed to extract diagnoses. Data from the two previous five-year periods were taken from institutional records. A univariate analysis was performed, along with calculation of absolute and relative frequencies for qualitative variables, and central tendency and dispersion measures for quantitative variables.
Results: The study collected the diagnoses of 1,171 patients, 51.8% (607) of whom were male, and 64% (753/1171), under five years of age. The main diagnoses were: constipation (33.9%), food allergy (23.5%), eating disorders (5.5%), gastroesophageal reflux disease (4.1%), peptic ulcer disease (4.1%), persistent diarrhea (3.8%) and cystic fibrosis (3.4%). Upon comparing this period with the two previous ones, we observed that peptic ulcer disease decreased while constipation, which was in the second position, rose to the first place. Food allergy, not registered within the first ten diagnoses in previous periods, appeared during this last period.
Conclusions: During the last five years, constipation was the first gastrointestinal diagnosis followed by food allergy, in agreement with the global trend. It is essential, therefore, to apply diagnostic algorithms, timely treatment, and prevention.
Downloads
References
Chey WD. The role of food in the functional gastrointestinal disorders: Introduction to a manuscript series. Am J Gastroenterol. 2013;108:694-7. https://doi.org/10.1038/ajg.2013.62
Mora D, Daza W, Dadán S. Comportamiento epidemiológico de las enfermedades digestivas pediátricas en una Unidad de Gastroenterología, Hepatología y Nutrición Pediátrica de Bogotá-Gastronutriped (1997-2006) (tesis). Bogotá: Universidad El Bosque; 2010.
Profamilia. Encuesta Nacional de Demografía y Salud – ENDS 2010. Bogotá: Printex Impresores; 2010. Fecha de consulta: 3 de agosto de 2016. Disponible en: https://dhsprogram.com/pubs/pdf/FR246/FR246.pdf
Ministerio de la Protección Social. Encuesta Nacional de Salud 2007. Resultados Nacionales. Bogotá, D.C.: Javegraf; 2009. Fecha de consulta: 3 de agosto de 2016. Disponible en: http://www.minsalud.gov.co/Documentos%20y%20Publicaciones/ENCUESTA%20NACIONAL.pdf
Baber KF, Anderson J, Puzanovova M, Walker LS. Rome II versus Rome III classification of functional gastrointestinal disorders in pediatric chronic abdominal pain. J Pediatr Gastroenterol Nutr. 2008;47:299-302. https://doi.org/10.1097/MPG.0b013e31816c4372
Zolezzi FA. Las enfermedades funcionales gastrointestinales y Roma III. Rev Gastroenterol Perú. 2007;27:177-84.
Altamimi E. Clinical characteristics of pediatric constipation in South Jordan. Pediatr Gastroenterol Hepatol Nutr. 2014;17:155-61. https://doi.org/10.5223/pghn.2014.17.3.155
Chu H, Zhong L, Li H, Zhang X, Zhang J, Hou X. Epidemiology characteristics of constipation for general population, pediatric population, and elderly population in China. Gastroenterol Res Pract. 2014;2014:1-12. https://doi.org/10.1155/2014/532734
Velasco CA. Actualización sobre estreñimiento crónico funcional en niños. Colomb Med. 2005;36:55-61.
Oliveira JN, Tahan S, Goshima S, Fagundes-Neto U, Morais MB. Prevalence of constipation in adolescents enrolled in São José dos Campos, SP, Brazil, schools and in their parents. Arq Gastroenterol. 2006;43:50-4. https://doi.org/10.1590/S0004-28032006000100013
Dehghani SM, Kulouee N, Honar N, Imanieh MH, Haghighat M, Javaherizadeh H. Clinical manifestations among children with chronic functional constipation. Middle East J Dig Dis. 2015;7:31-5.
Daza W, Dadán S. Estreñimiento. En: Leal FJ, editor. El pediatra eficiente. Séptima edición. Bogotá: Editorial Médica Panamericana; 2013. p. 436-53.
Everhart JE, Ruhl CE. Burden of digestive diseases in the United States part II: lower gastrointestinal diseases. Gastroenterology 2009; 36:741-54.
Karami H, Shokohi L. Management of childhood constipation. J Pediatr Rev. 2013;1:45-51.
Rajindrajith S, Devanarayana NM. Constipation in children: Novel insight into epidemiology, pathophysiology and management. J Neurogastroenterol Motil. 2011;17:35-47. https://doi.org/10.5056/jnm.2011.17.1.35
Comberiati P, Cipriani F, Schwarz A, Posa D, Host C, Peroni DG. Diagnosis and treatment of pediatric food allergy: An update. Ital J Pediatr. 2014;41:13. https://doi.org/10.1186/s13052-014-0108-0
Keet CA, Savage JH, Seopaul S, Peng RD, Wood RA, Matsui EC. Temporal trends and racial/ethnic disparity in self-reported pediatric food allergy in the United States. Ann Allergy Asthma Immunol. 2014;112:222-9. https://doi.org/10.1016/j.anai.2013.12.007
Sicherer SH, Sampson HA. Food allergy: Epidemiology, pathogenesis, diagnosis, and treatment. J Allergy Clin Immunol. 2014;133:291-307. https://doi.org/10.1016/j.jaci.2013.11.020
Saito AM. Alergia e intolerancia alimentaria, manifestaciones gastrointestinales. Rev Peru Pediatr. 2007;60:111-7.
Lifschitz C, Szajewska H. Cow’s milk allergy: Evidencebased diagnosis and management for the practitioner. Eur J Pediatr. 2015;174:141-50. https://doi.org/10.1007/s00431-014-2422-3
Boye JI. Food allergies in developing and emerging economies: Need for comprehensive data on prevalence rates. Clin Transl Allergy. 2012;25:1-9. https://doi.org/10.1186/2045-7022-2-25
Daza W, Dadán S, Rojas A. Alergia alimentaria en la infancia. Revista de educación continua de la Sociedad Colombiana de Pediatría. 2014;3:49-58. Fecha de consulta: 11 de marzo de 2016. Disponible en: https://scp.com.co/precop-old/pdf/3_5.pdf
Searing DA, Leung D. Vitamin D in atopic dermatitis, asthma and allergic diseases. Immunol Allergy Clin North Am. 2010;30:397-409. https://doi.org/ 10.1016/j.iac.2010.05.005
Liu X, Arguelles L, Zhou Y, Wang G, Chen Q, Tsai HJ, et al. The longitudinal trajectory of vitamin D status from birth to early childhood on the development of food sensitization. Pediatr Res. 2013;74:321-6. https://doi.org/10.1038/pr.2013.110
Bravo P, Hodgson MI. Trastornos alimentarios del lactante y preescolar. Rev Chil Pediatr. 2011;82:87-92. https://doi.org/10.4067/S0370-41062011000200002
Kerzner B, Milano K, MacLean WC, Berall G, Stuart S, Chatoor I. A practical approach to classifying and managing feeding difficulties. Pediatrics. 2015;135:344-53. https://doi.org/10.1542/peds.2014-1630
Meyer R, Rommel N, van Oudenhove L, Fleming C, Dziubak R, Shah NJ. Feeding difficulties in children with food protein-induced gastrointestinal allergies. Gastroenterol Hepatol. 2014;29:1764-9. https://doi.org/10.1111/jgh.12593
Harris RF, Menard-Katcher C, Atkins D, Furuta GT, Klinnert MD. Psychosocial dysfunction in children and adolescents with eosinophilic esophagitis. J Pediatr Gastroenterol Nutr. 2013;57:500-5. https://doi.org/10.1097/MPG.0b013e31829ce5ad
Mukkada VA, Haas A, Maune NC, Capocelli KE, Henry M, Gilman N, et al. Feeding dysfunction in children with eosinophilic gastrointestinal diseases. Pediatrics. 2010;126:672-7. https://doi.org/10.1542/peds.2009-2227
Esposito C, Roberti A, Escolino M, Cerulo M, Settimi A, Farina A, et al. Management of gastroesophageal reflux disease in pediatric patients: A literature review. Pediatric Health Med Ther. 2015;6:1-8. https://dx.doi.org/10.2147/PHMT.S46250
Zagorski S, Nazarenko O. Reflux esophagitis and Helicobacter pylori: Is there an association in children? Prog Health Sci. 2014;4:41-6.
Uribe-Garay C. Enfermedad ácido péptica en la infancia. Bogotá, D.C.: Sociedad Colombiana de Pediatría; 2014. p. 37-48. Fecha de consulta: 3 de agosto de 2016. Disponible en: https://scp.com.co/precop-old/pdf/3_4.pdf
Tabbers MM, DiLorenzo C, Berger MY, Faure C, Langendam MW, Nurko S, et al. Evaluation and treatment of functional constipation in infants and children: Evidencebased recommendations from ESPGHAN and NASPGHAN. J Pediatr Gastroenterol Nutr. 2014;58:258-74. https://doi.org/10.1097/MPG.0000000000000266
Some similar items:
- Ángela M. Pedraza, Carlos E. Rodríguez-Martínez, Ranniery Acuña, Initial validation of a scale to measure the burden for parents/caregivers of children with asthma and factors associated with this burden in a population of asthmatic children , Biomedica: Vol. 33 No. 3 (2013)
- Marcela González, Claudia Patricia González, Alvaro Sanabria, Ultrasonographic estimation of the normal volume of the thyroid gland in pediatric populations. , Biomedica: Vol. 26 No. 1 (2006)
- Luisa F. Imbachi, Lina M. Ibañez , Paula Hurtado-Villa, Health status and barriers in health care for children with birth defects born between 2011 and 2017 in two institutions in Cali , Biomedica: Vol. 40 No. 1 (2020)
- Tania Yadira Martínez-Rodríguez, Mauricio Rey-Buitrago, Alpha sinuclein expression in blood and its relationship with chronic constipation in a population from Bogotá, D.C., with problems of alcohol consumption , Biomedica: Vol. 40 No. 2 (2020)
- Freddy Israel Pantoja, Willinton Robert Ricaurte , Diana Elizabeth Rosero , Relationship between death and admission of pediatric patients to intensive care due to Staphylococcus aureus bacteremia acquired in the community, 2014-2017 , Biomedica: Vol. 41 No. 1 (2021)
- Yesica Llimpe, Cytogenetic risk groups for childhood acute myeloid leukemia based on survival analysis in a cancer referral hospital from Perú , Biomedica: Vol. 41 No. 2 (2021)
- Jorge Andrés Puerto, Susana Uribe , Víctor Calvo, Ricardo Cardona, Impact of the allergen-specific immunotherapy in pediatric patients with asthma treated at a health institution in Colombia , Biomedica: Vol. 41 No. 3 (2021)
- Miguel Ángel Medina, Wendy Meyer , Carolina Echeverri , Natalia Builes , Langerhans cell histiocytosis: Case report and literature review , Biomedica: Vol. 41 No. 3 (2021)
- Luis Carlos Salazar, Luz Ángela Moreno , Lina Eugenia Jaramillo , Edgar Vladimir Cabrera , Erdheim-Chester disease: First pediatric case report in Colombia , Biomedica: Vol. 41 No. 4 (2021)
- Natalia Vélez-Tirado , Lina Castaño-Jaramillo , Sonia Restrepo-Gualteros , Catalina Alcalá-Lozano, Erika Ruge , Carolina Puente , Diana Li-Zeng , Diego Chaparro-Arce , María Camila Beltrán-Dimas , Juan Francisco López , Miguel Luengas-Monroy , Diego Galvis-Trujillo , Iván Gutiérrez-Tobar , Pablo Vásquez-Hoyos , Germán Camacho-Moreno , Severe adenovirus infection outbreak in Colombia: Experience from a tertiary pediatric hospital in 2022 , Biomedica: Vol. 44 No. 1 (2024)
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























