Mucosal leishmaniasis: A forgotten disease, description and identification of species in 50 Colombian cases
Abstract
Introduction: Mucosal leishmaniasis has a progressive course and can cause deformity and even mutilation in the affected areas. It is endemic in the American continent and it is mainly caused by Leishmania (Viannia) braziliensis.
Objective: To describe a series of mucosal leishmaniasis cases and the infectious Leishmania species.
Materials and methods: We included 50 patients with a clinical diagnosis of mucosal leishmaniasis and parasitological confirmation, and we described their clinical and laboratory results. We performed species typing by PCR-RFLP using the miniexon sequence and hsp70 genes; confirmation was done by sequencing.
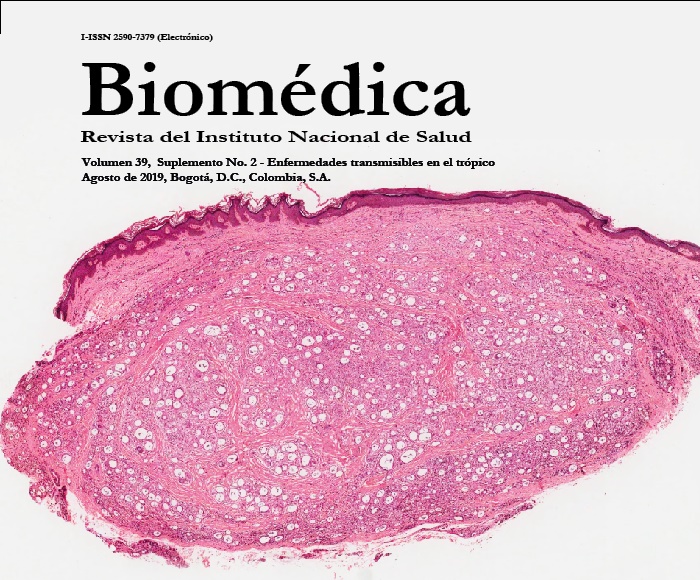
Results: The median time of disease evolution was 2.9 years (range: 1 month to 16 years). The relevant clinical findings included mucosal infiltration (94%), cutaneous leishmaniasis scar (74%), total loss of the nasal septum (24%), nasal deformity (22%), and mucosal ulceration (38%). The symptoms reported included nasal obstruction (90%), epistaxis (72%), rhinorrhea (72%), dysphonia (28%), dysphagia (18%), and nasal pruritus (34%). The histopathological study revealed a pattern compatible with leishmaniasis in 86% of the biopsies, and amastigotes were identified in 14% of them. The Montenegro skin test was positive in 86% of patients, immunofluorescence in 84%, and culture in 8%. Leishmania (V.) braziliensis was identified in 88% of the samples, L. (V) panamensis in 8%, and L. (V.) guyanensis and L. (L.) amazonensis in 2% respectively.
Conclusion: In this study, we found a severe nasal disease with destruction and deformity of the nasal septum in 25% of the cases, probably associated with late diagnosis. Leishmania (V.) braziliensis was the predominant species. We described a case of mucosal leishmaniasis in Colombia caused by L. (L.) amazonensis for the first time.
Downloads
References
de Oliveira CI, Brodskyn CI. The immunobiology of Leishmania braziliensis infection. Front Inmunol. 2012;3:145. https://doi.org/10.3389/fimmu.2012.00145
Lessa HA, Lessa MM, Guimarães LH, Lima CM, Arruda S, Machado PR, et al. A proposed new clinical staging system for patients with mucosal leishmaniasis. Trans R Soc Trop Med Hyg. 2012;160:376-81. https://doi.org/10.1016/j.trstmh.2012.03.007
Strazzulla A, Cocuzza S, Pinzone MR, Postorino MC, Consentino C, Serra A, et al. Mucosal leishmaniasis: An underestimated presentation of a neglected disease. Biomed Res Int. 2013:1-7. https://doi.org/10.1155/2013/805108
Amato VS, Toun FF, Bacha HA, Neto VA, Nicodemo AC. Mucosal leishmaniasis current scenario and prospects for treatment. Acta Trop. 2008;105:1-9. https://doi.org/10.1016/j.actatropica.2007.08.003
Guerra J.A, Prestes SR, Silveira H, Coelho LI, Gama P, Moura A, et al. Mucosal leishmaniasis caused by Leishmania (Viannia) braziliensis and Leishmania (Viannia) guyanensis in the Brazilian Amazon. Plos Negl Trop Dis. 2011;5:e980. https://doi.org/10.1371/journal.pntd.0000980
Osorio LE, Castillo CM, Ochoa MT. Mucosal leishmaniasis due to Leishmania (Viannia) panamensis in Colombia: Clinical characteristics. Am J Trop Med Hyg. 1998;59:49-52. https://doi.org/10.4269/ajtmh.1998.59.49
Ovalle‐Bracho C, Díaz‐Toro YR, Muvdi‐Arenas S. Polymerase chain reaction–miniexon: A promising diagnostic method for mucocutaneous leishmaniasis. Int J Dermatol. 2016;55:531-9. https://doi.org/10.1111/ijd.12910
Marfurt J, Nasereddin A, Niederwieser I, Jaffe CL, Beck HP, Felger I. Identification and differentiation of Leishmania species in clinical samples by PCR amplification of the miniexon sequence and subsequent restriction fragment length polymorphism analysis. J Clin Microbiol. 2003;41:3147-53. https://doi.org/10.1128/JCM.41.7.3147-3153.2003
Diniz JL, Costa MO, Gonçalves DU. Mucocutaneus leishmaniasis: Clinical markers in presumptive diagnosis. Braz J Otorhinolaryngol. 2011; 77:380-4. https://doi.org/10.1590/S1808-86942011000300018
Marsden PD. Mucosal leishmaniasis (“espundia” Escomel, 1911). Trans R Soc Trop Med Hyg. 1986; 802:859-79. https://doi.org/10.1016/0035-9203(86)90243-9
Passos VM, Barreto SM, Romanha AJ, Krettli AU, Volpini AC, Gontijo CM, et al. Cutaneous leishmaniasis in the Metropolitan Region of Belo Horizonte: Clinical, laboratorial, therapeutic and prospective aspects. Rev Soc Bras Med Trop. 2001; 34:5-12. https://doi.org/10.1590/S0037-86822001000100002
Boaventura VS, Café V, Costa J, Oliveira F, Bafica A, Rosato A, et al. Short report: Concomitant early mucosal and cutaneous leishmaniasis in Brazil. Am J Trop Med Hyg. 2006; 75:267-69. https://doi.org/10.4269/ajtmh.2006.75.267
Marsden PD. Clinical presentations of Leishmaniasis braziliensis braziliensis. Parasitol Today. 1985; 1:129-33. https://doi.org/10.1016/0169-4758(85)90057-2
Sáenz RE, de Rodríguez CG, Johnson CM, Berman JD. Efficacy and toxicity of pentostam against leishmaniasis. Am J Trop Med Hyg 1991;44:394-8. https://doi.org/10.4269/ajtmh.1991.44.394
Llanos-Cuentas EA, Cuba CC, Barreto AC, Magalhaes AV, Lago EL, Reed SG, et al. Human mucocutaneous leishmaniasis in Tres Braços, Bahía – Brazil. An area of Leishmania braziliensis braziliensis transmission. I. Laboratory diagnosis. Rev Soc Bras Med Trop. 1984;17:161-7. https://doi.org/10.1590/S0037-86821984000400002
Lessa MM, Lessa HA, Castro TW, Oliveira A, Scherifer A, Machado P, et al. Mucosal leishmaniasis: Epidemiological and clinical aspects. Braz J Otorhinolaryngol. 2007;73:843-7. https://doi.org/10.1016/S1808-8694(15)31181-2
Azambuja RR, Sampadio RN, Marsden PD. Current aspects of endemic mucocutaneous leishmaniasis in Brazil. Hautarzt. 1985;36:531-3.
Cantanhede LM, da Silva CF, Ito MM, Felipin KP, Nicolete R, Villalobos JM, et al. Further evidence of an association between the presence of Leishmania RNA virus 1 and the mucosal manifestations in tegumentary leishmaniasis patients. Plos Negl. Trop. Dis. 2015;9:e0004079. https://doi.org/10.1371/journal.pntd.0004079
Kharfi M, Benmously R, El Fekih N, Daoud M, Fitouri Z, Mokhtar I. et al. Childhood leishmaniasis: Report of 106 cases. Dermatol Online J. 2004;10:6. https://doi.org/10.3347/kjp.2006.44.4.355
Guerra JA, Barbosa MD, Loureiro AC, Coelho CP, Rosa GG, Coelho LI. American tegumentary leishmaniasis in children: Epidemiological aspects of cases treated in Manaus, Amazonas, Brazil. Cad Saúde Pública. 2007;23:2215-23. https://doi.org/10.1590/S0102-311X2007000900029
Some similar items:
- Clemencia Ovalle-Bracho, Carolina Camargo, Yira Díaz-Toro, Marcela Parra-Muñoz, Molecular typing of Leishmania (Leishmania) amazonensis and species of the subgenus Viannia associated with cutaneous and mucosal leishmaniasis in Colombia: A concordance study , Biomedica: Vol. 38 No. 1 (2018)
- Johana Marin, Daniel Urrea, Carlos Muskus, María Clara Echeverry, Ana María Mejía, Omar Triana, High-resolution melting analysis based on specific genomic regions: A promising tool for the diagnosis and typing of species causing cutaneous leishmaniasis in Colombia , Biomedica: Vol. 37 No. 4 (2017)
- Jazzmín Arrivillaga-Henríquez, Sandra Enríquez, Vanessa Romero, Gustavo Echeverría, Jorge Pérez-Barrera, Ana Poveda, Juan-Carlos Navarro, Alon Warburg, Washington Benítez, Eco-epidemiological aspects, natural detection and molecular identification of Leishmania spp. in Lutzomyia reburra, Lutzomyia barrettoi majuscula and Lutzomyia trapidoi , Biomedica: Vol. 37 No. Sup. 2 (2017): Suplemento 2, Entomología médica, 2017
- Ana Margarita Montalvo, Lianet Monzote, Jorge Fraga, Ivón Montano, Carlos Muskus, Marcel Marín, Simonne De Donck, Iván Darío Vélez, Jean Claude Dujardin, PCR-RFLP and RAPD for typing neotropical Leishmania , Biomedica: Vol. 28 No. 4 (2008)
- Marcel Marín, Yudy Alexandra Aguilar, José Robinson Ramírez, Omar Triana, Carlos Enrique Muskus, Molecular and immunological analyses suggest the absence of hydrophilic surface proteins in Leishmania (Viannia) panamensis , Biomedica: Vol. 28 No. 3 (2008)
- Ana M. Montalvo, Jorge Fraga, Ivón Montano, Lianet Monzote, Gert Van der Auwera, Marcel Marín, Carlos Muskus, Molecular identification of Leishmania spp. clinical isolates from Colombia based on hsp70 gene , Biomedica: Vol. 36 (2016): Suplemento 1, Microbiología médica
- Mercedes Salcedo-Cifuentes, Jesús Cabrera, Yesid Cuesta-Astroz, Edwin Carrascal, Yoshito Eizuru, Martha C. Domínguez, Adalberto Sánchez, Felipe García-Vallejo, Clonal expansion and genomic characterization of the human T-cell lymphotropic virus type I during the integration process in adult T-cell leukemia/lymphoma , Biomedica: Vol. 29 No. 2 (2009)
- Nora Cardona-Castro, Lelia Lavalett, Miryan Margot Sánchez, Nélida Múñoz, Jaime Moreno, Development and validation of a multiplex polymerase chain reaction for molecular identification of Salmonella enterica serogroups B, C2, D and E , Biomedica: Vol. 29 No. 2 (2009)
- Diego Fernando Zea, Martín Prager, Roger Adrian Figueroa, María Consuelo Miranda, Mucosal complication of cutaneous leishmaniasis , Biomedica: Vol. 29 No. 1 (2009)
- Concepción Judith Puerta, Johana María Guevara, Paula Ximena Pavía, Marleny Montilla, Rubén Santiago Nicholls, Edgar Parra, Yuli Katherine Barrera, Evaluation of TcH2AF-R and S35-S36 primers in PCR tests for the detection of Trypanosoma cruzi in mouse cardiac tissue , Biomedica: Vol. 28 No. 4 (2008)
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























