Leptospirosis and rickettsiosis, a diagnostic challenge for febrile syndrome in endemic areas
Abstract
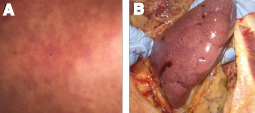
This is the case of a 50-year-old male from the region of Urabá, Colombia, with a mixed infection by Rickettsia rickettsii and Leptospira interrogans serovar Copenhageni ST78 and negative test for malaria and dengue fever.
The patient presented with febrile syndrome and was unresponsive to systemic antibiotic treatment, who finally died in the intensive care unit. We established the postmortem diagnosis through molecular typification of the two etiological agents. In the inspection at the patient’s home, we found a Rattus rattus specimen infected with L. interrogans of the same serovar found in him. We found no ticks parasitizing the domestic animals cohabitating with the patient.
This case of a mixed infection with progressive and fatal symptoms in a patient with occupational risk in a tropical disease endemic zone highlights the importance of considering the potential presentation of simultaneous etiologies in patients with multiple medical visits for unresolved febrile syndromes associated with risky exposure during agricultural activities.
Downloads
References
Karnad DR, Richards GA, Silva GS, Amin P, Council of the World Federation of Societies of Intensive and Critical Care Medicine. Tropical diseases in the ICU: A syndromic approach to diagnosis and treatment. J Crit Care. 2018;46:119-26. https://doi.org/10.1016/j.jcrc.2018.03.025
Kothari VM, Karnad DR, Bichile LS. Tropical infections in the ICU. J Assoc Physicians India. 2006;54:291-8.
Montenegro DC, Bitencourth K, de Oliveira SV, Borsoi AP, Cardoso KM, Sousa MS, et al. Spotted fever: Epidemiology and vector-rickettsia-host relationship in Rio de Janeiro State. Front Microbiol. 2017;8:505. https://doi.org/10.3389/fmicb.2017.00505
Chin Vk, Lee TY, Lim WF, Wan Shahriman YW, Syafinaz AN, Zamberi S, et al. Leptospirosis in human: Biomarkers in host immune responses. Microbiol Res. 2018;207:108-15. https://doi.org/10.1016/j.micres.2017.11.015
Mattar S, Tique V, Miranda J, Montes E, Garzón D. Undifferentiated tropical febrile illness in Córdoba, Colombia: Not everything is dengue. J Infect Public Health. 2017;10:507-12. https://doi.org/10.1016/j.jiph.2016.09.014
Arroyave E, Londoño AF, Quintero JC, Agudelo-Flórez P, Arboleda M, Díaz FJ, et al. Etiología y caracterización epidemiológica del síndrome febril no palúdico en tres municipios del Urabá antioqueño, Colombia. Biomédica. 2013;33(Supl.1):99-107. https://doi.org/10.7705/biomedica.v33i0.734
Martínez-Caballero A, Moreno B, González C, Martínez G, Adames M, Pachar JV, et al. Descriptions of two new cases of Rocky Mountain spotted fever in Panama, and coincident infection with Rickettsia rickettsii in Rhipicephalus sanguineus s.l. in an urban locality of Panama City, Panama. Epidemiol Infect. 2018;146:875-8.
https://doi.org/10.1017/S0950268818000730
Wang H-K, Lee M-H, Chen Y-C, Hsueh P-R, Chang S-C. Factors associated with severity and mortality in patients with confirmed leptospirosis at a regional hospital in northern Taiwan. J Microbiol Immunol Infect. 2020;53:307-14. https://doi.org/10.1016/j.jmii.2018.05.005
Vikram K, Agarwala P, Bhargava A, Jain Y, Jagzape T, Wasnik P. Scrub typhus and leptospirosis in rural and urban settings of central India: A preliminary evaluation. Trop Doct. 2020;50:111-5. https://doi.org/10.1177/0049475519889712
Quintero JC, Paternina LE, Uribe A, Muskus C, Hidalgo M, Gil J, et al. Eco-epidemiological analysis of rickettsial seropositivity in rural areas of Colombia: A multilevel approach. PLoS Negl Trop Dis. 2017;11:e0005892. https://doi.org/10.1371/journal.pntd.0005892
Peláez-Sanchez RG, López JÁ, Pereira MM, Arboleda-Naranjo M, Agudelo-Flórez P. Genetic diversity of Leptospira in northwestern Colombia: First report of Leptospira santarosai as a recognized leptospirosis agent. Mem Inst Oswaldo Cruz. 2016;111:737-44. https://doi.org/10.1590/0074-02760160245
Boonsilp S, Thaipadungpanit J, Amornchai P, Wuthiekanun V, Bailey MS, Holden MTG, et al. A single multilocus sequence typing (MLST) scheme for seven pathogenic Leptospira species. PLoS Negl Trop Dis. 2013;7:e1954. https://doi.org/10.1371/journal.pntd.0001954
Ahmed N, Devi SM, Valverde M de los A, Vijayachari P, Machang’u RS, Ellis WA, et al. Multilocus sequence typing method for identification and genotypic classification of pathogenic Leptospira species. Ann Clin Microbiol Antimicrob. 2006;5:28. https://doi.org/10.1186/1476-0711-5-28
Londoño AF, Acevedo-Gutiérrez LY, Marín D, Contreras V, Díaz FJ, Valbuena G, et al. Human prevalence of the spotted fever group (SFG) rickettsiae in endemic zones of Northwestern Colombia. Ticks Tick-Borne Dis. 2017;8:477-82. https://doi.org/10.1016/j.ttbdis.2017.02.006
Ko AI, Goarant C, Picardeau M. Leptospira: The dawn of the molecular genetics’ era for an emerging zoonotic pathogen. Nat Rev Microbiol. 2009;7:736-47. https://doi.org/10.1038/nrmicro2208
De Brito T, Silva AMG da, Abreu PAE. Pathology and pathogenesis of human leptospirosis: A commented review. Rev Inst Med Trop Sao Paulo. 2018;60:e23. https://doi.org/10.1590/s1678-9946201860023
Parola P, Paddock CD, Socolovschi C, Labruna MB, Mediannikov O, Kernif T, et al. Update on tick-borne rickettsioses around the world: A geographic approach. Clin Microbiol Rev. 2013; 26:657-702. https://doi.org/10.1128/CMR.00032-13
Quintero-Vélez JC, Faccini-Martínez ÁA, Rodas-González JD, Díaz FJ, Ramírez-García R, Somoyar-Ordosgoitia P, et al. Fatal Rickettsia rickettsii infection in a child, Northwestern Colombia, 2017. Ticks Tick-Borne Dis. 2019;10:995-6. https://doi.org/10.1016/j.ttbdis.2019.05.009
Jaramillo L, Arboleda M, García V, Agudelo-Flórez P. Coinfección brucelosis-leptospirosis, Urabá, Colombia. Reporte de caso. Infectio. 2014;18:72-6. https://doi.org/10.1016/j.infect.2014.02.002
Prabhakar U, Singh A. Atypical presentation of rickettsial spotted fever. J Ayub Med Coll Abbottabad. 2017;29:692-3.
Licona-Enriquez JD, Delgado-de la Mora J, Paddock CD, Ramírez-Rodríguez CA, Candia-Plata MDC, Hernández GÁ. Rocky mountain spotted fever and pregnancy: Four cases from Sonora, México. Am J Trop Med Hyg. 2017;97:795-8. https://doi.org/10.4269/ajtmh.16-0917
Cagliero J, Villanueva SYAM, Matsui M. Leptospirosis pathophysiology: Into the storm of cytokines. Front Cell Infect Microbiol. 2018;8:204. https://doi.org/10.3389/fcimb.2018.00204
Bhavnani SK, Drake J, Bellala G, Dang B, Peng B-H, Oteo JA, et al. How cytokines co-occur across rickettsioses patients: From bipartite visual analytics to mechanistic inferences of a cytokine storm. AMIA Jt Summits Transl Sci Proc. 2013;18:2013:15-9.
Some similar items:
- Piedad Agudelo-Flórez, Marcos Restrepo, Natalí Moreno, Diagnosis of leptospirosis by dark-field microscopy of blood samples and culture , Biomedica: Vol. 28 No. 1 (2008)
- Carolina Gómez, Ruth María Eraso, Carlos A. Aguirre, María del Pilar Pérez, Kikuchi-Fujimoto disease: pediatric case presentation , Biomedica: Vol. 30 No. 4 (2010)
- Álvaro A. Faccini-Martínez, Elkin G. Forero-Becerra, Jesús A. Cortés-Vecino, Luis J. Polo-Teran, Jorge H. Jácome, Jimmy J. Vargas, Gustavo Valbuena, Marylin Hidalgo, Probable case of flea-borne spotted fever (Rickettsia felis) , Biomedica: Vol. 33 (2013): Suplemento 1, Fiebres hemorrágicas
- Jefferson Antonio Buendía, Juana Patricia Sánchez-Villamil, Gabriela Urman, Cost-effectiveness of diagnostic strategies of severe bacterial infection in infants with fever without a source , Biomedica: Vol. 36 No. 3 (2016)
- Fernando Rosso, Sara Vanegas, Sarita Rodríguez, Robinson Pacheco, Prevalence and clinical course of dengue infection in elderly patients with acute febrile illness in a tertiary care hospital in Cali, Colombia , Biomedica: Vol. 36 (2016): Suplemento 2, Enfermedades virales
- Eliana Patricia Calvo, Carolina Coronel-Ruiz, Syrley Velazco, Myriam Velandia-Romero, Jaime E. Castellanos, Dengue and Chikungunya differential diagnosis in pediatric patients , Biomedica: Vol. 36 (2016): Suplemento 2, Enfermedades virales
- Jorge Cedano, Sarita Rodríguez, Winy Kujundzic, Juan Sebastián Arana, Robinson Pacheco, Fernando Rosso, Clinical characterization of patients with severe leptospirosis in a tertiary hospital in Cali, Colombia, 2010-2016 , Biomedica: Vol. 39 No. Sp. 1 (2019): Suplemento 1, Microbiología médica, mayo
- Julio César Martínez, Claudia Llerena, Yanely Angélica Valbuena, The Importance of investigating Mycobacterium bovis in clinical samples of human origin , Biomedica: Vol. 39 No. Sp. 1 (2019): Suplemento 1, Microbiología médica, mayo
- Byron Flores, Nabil Halaihel , Tania Pérez-Sánchez , Jessica Sheleby-Elías , Brenda Mora , Héctor Fuertes , William Jirón , Evaluation of three qPCR for the detection of pathogenic leptospires in domestic animals in Nicaragua , Biomedica: Vol. 40 No. 4 (2020)
- Nancy Y. Angulo , Paula A. Castaño, Crhistian C. Gómez , Santiago Quintero , Neuroleptic malignant syndrome associated with acute organophosphate poisoning: Case report , Biomedica: Vol. 42 No. 3 (2022)
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























