Update of antimicrobial resistance in level III and IV health institutions in Colombia between January 2018 and December 2021
Abstract
Introduction. Antimicrobial resistance surveillance is a fundamental tool for the development, improvement, and adjustment of antimicrobial stewardship programs,
therapeutic guidelines, and universal precautions to limit the cross-transmission of resistant bacteria between patients. Since the beginning of 2020, the SARS-CoV-2 pandemic profoundly challenged the health system and, according to some reports, increased the rates of antimicrobial resistance.
Objective. To describe the behavior of antimicrobial resistance of the most frequent bacterial pathogens in twenty Colombian hospitals from January 2018 to December 2021.
Materials and methods. We conducted a descriptive study based on the microbiological information recorded from January 2018 to December 2021 in twenty levels III and IV health institutions in twelve Colombian cities. We identified the species of the ten most frequent bacteria along with their resistance profile to the antibiotic markers after analyzing the data through WHONET.
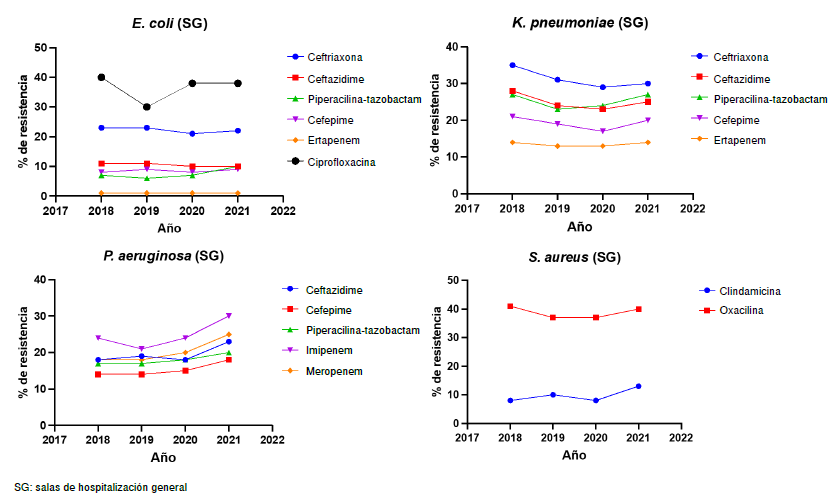
Results. We found no statistically significant changes in most pathogens’ resistance profiles from January 2018 to December 2021. Only Pseudomonas aeruginosa had
a statistically significant increase in its resistance profile, particularly to piperacillin/tazobactam and carbapenems.
Conclusions. The changes in antimicrobial resistance in these four years were not statistically significant except for P. aeruginosa to piperacillin/tazobactam and carbapenems.
Downloads
References
Haustein T, Gastmeier P, Holmes A, Lucet JC, Shannon RP, Pittet D, et al. Use of benchmarking and public reporting for infection control in four high-income countries. Lancet Infect Dis. 2011;11:471-81. https://doi.org/10.1016/S1473-3099(10)70315-7
World Health Organization. Guidelines for the prevention and control of carbapenemresistant Enterobacteriaceae, Acinetobacter baumannii and Pseudomonas aeruginosa in health care facilities. Geneva: World Health Organization; 2017.
Lan P, Jiang Y, Zhou J, Yu Y. A global perspective on the convergence of hypervirulence and carbapenem resistance in Klebsiella pneumoniae. J Glob Antimicrob Resist. 2021;25:26-34. https://doi.org/10.1016/j.jgar.2021.02.020
Critchley IA, Karlowsky JA. Optimal use of antibiotic resistance surveillance systems. Clin Microbiol Infect. 2004;10:502-11. https://doi.org/10.1111/j.1469-0691.2004.00911.x
Harbarth S, Balkhy HH, Goossens H, Jarlier V, Kluytmans J, Laxminarayan R, et al. Antimicrobial resistance: One world, one fight! Antimicrob Resist Infect Control. 2015;4:1-15. https://doi.org/10.1186/s13756-015-0091-2
Castanheira M, Deshpande LM, Mendes RE, Canton R, Sader HS, Jones RN. Variations in the occurrence of resistance phenotypes and carbapenemase genes among Enterobacteriaceae isolates in 20 years of the SENTRY antimicrobial surveillance program. Open Forum Infect Dis. 2019;6(Suppl.1):S23-33. https://doi.org/10.1093/ofid/ofy347
Paterson DL, Rossi F, Baquero F, Hsueh PR, Woods GL, Satishchandran V, et al. In vitro susceptibilities of aerobic and facultative Gram-negative bacilli isolated from patients with intra-abdominal infections worldwide: The 2003 Study for Monitoring Antimicrobial Resistance Trends (SMART). Int J Antimicrob Agents. 2005;55:965-73. https://doi.org/10.1093/jac/dki117
Canton R, Gijon D, Ruiz-Garbajosa P. Antimicrobial resistance in ICUs: An update in the light of the COVID-19 pandemic. Curr Opin Crit Care. 2020;26:433-41. https://doi.org/10.1097/MCC.0000000000000755
Shortridge D, Gales AC, Streit JM, Huband MD, Tsakris A, Jones RN. Geographic and temporal patterns of antimicrobial resistance in pseudomonas aeruginosa over 20 years from the SENTRY Antimicrobial Surveillance Program, 1997-2016. Open Forum Infect Dis. 2019;6(Suppl.1):S63-8. https://doi.org/10.1093/ofid/ofy343
Segala FV, Bavaro DF, Di Gennaro F, Salvati F, Marotta C, Saracino A, et al. Impact of sars-cov-2 epidemic on antimicrobial resistance: A literature review. Viruses. 2021;13:1-15. https://doi.org/10.3390/v13112110
Jeon K, Jeong S, Lee N, Park MJ, Song W, Kim HS, et al. Impact of COVID-19 on antimicrobial consumption and spread of multidrug-resistance in bacterial infections. Antibiotics. 2022;11:1-12. https://doi.org/10.3390/antibiotics11040535
Kariyawasam RM, Julien DA, Jelinski DC, Larose SL, Rennert-May E, Conly JM, et al. Antimicrobial resistance (AMR) in COVID-19 patients: A systematic review and metaanalysis (November 2019–June 2021). Antimicrob Resist Infect Control. 2022;11. https://doi.org/10.1186/s13756-022-01085-z
Hughes S, Troise O, Donaldson H, Mughal N, Moore LSP. Bacterial and fungal coinfection among hospitalised patients with COVID-19. Clin Microbiol Infect. 2020;26:1395-9. https://doi.org/10.1016/j.cmi.2020.06.025
van Duin D, Barlow G, Nathwani D. The impact of the COVID-19 pandemic on antimicrobial resistance: A debate. JAC Antimicrob Resist. 2020;2:4-5. https://doi.org/10.1093/jacamr/dlaa053
Bork JT, Leekha S, Claeys K, Seung H, Tripoli M, Amoroso A, et al. Change in hospital antibiotic use and acquisition of multidrug-resistant gram-negative organisms after the onset of coronavirus disease 2019. Infect Control Hosp Epidemiol. 2021;42:1115-7. https://doi.org/10.1017/ice.2020.1360
Russo A, Gavaruzzi F, Ceccarelli G, Borrazzo C, Oliva A, Alessandri F, et al. Multidrugresistant Acinetobacter baumannii infections in COVID-19 patients hospitalized in intensive care unit. Infection. 2022;50:83-92. https://doi.org/10.1007/s15010-021-01643-4
Khojasteh S, Jafarzdeh J, Hosseini SA, Haghani I, Turki H, Aghaei Gharehbolagh S, et al. Candida auris and COVID-19: A health threatening combination. Curr Med Mycol. 2022;8:44-50. https://doi.org/10.18502/cmm.8.3.11211
Patel A, Emerick M, Cabunoc MK, Williams MH, Preas MA, Schrank G, et al. Rapid spread and control of multidrug-resistant Gram-negative bacteria in COVID-19 patient care units. Emerg Infect Dis. 2021;27:1234-7. https://doi.org/10.3201/eid2704.204036
Stelling JM, O’Brien TF. Surveillance of antimicrobial resistance: The WHONET program. Clin Infect Dis. 1997;24(Suppl.1):S157-68. https://doi.org/10.1093/clinids/24.supplement_1.s157
Clinical and Laboratory Standards Institute (CLSI). Performance standards for antimicrobial susceptibility testing. 32nd edition. Wayne, PA: Clinical and Laboratory Standards Institute; 2022.
Clinical and Laboratory Standards Institute (CLSI). Analysis and presentation of cumulative antimicrobial susceptibility test data; Approved guideline –Fourth edition. CLSI document M39-A4. Wayne, PA: Clinical and Laboratory Standards Institute; 2014.
Plante JA, Mitchell BM, Plante KS, Debbink K, Weaver SC, Menachery VD. The variant gambit: COVID-19’s next move. Cell Host Microbe. 2021;29:508-15. https://doi.org/10.1016/j.chom.2021.02.020
Ovalle MV, Saavedra SY, González MN, Hidalgo AM, Duarte C, Beltrán M. Resultados de la vigilancia nacional de la resistencia antimicrobiana de enterobacterias y bacilos Gram negativos no fermentadores en infecciones asociadas a la atención de salud, Colombia, 2012-2014. Biomédica. 2017;37:473-85. https://doi.org/10.7705/biomedica.v37i4.3432
Martínez-Guerra BA, González-Lara MF, de León-Cividanes NA, Tamez-Torres KM, Román-Montes CM, Rajme-López S, et al. Antimicrobial resistance patterns and antibiotic use during hospital conversion in the COVID-19 pandemic. Antibiotics. 2021;10:1-9. https://doi.org/10.3390/antibiotics10020182
Nowak MD, Sordillo EM, Gitman MR, Paniz Mondolfi AE. Coinfection in SARS-CoV-2 infected patients: Where are influenza virus and rhinovirus/enterovirus? J Med Virol. 2020;92:1699-700. https://doi.org/10.1002/jmv.25953
Maes M, Higginson E, Pereira-Dias J, Curran MD, Parmar S, Khokhar F, et al. Ventilatorassociated pneumonia in critically ill patients with COVID-19. Crit Care. 2021;25:1-11. https://doi.org/10.1186/s13054-021-03460-5
Briceño DF, Correa A, Valencia C, Torres JA, Pacheco R, Montealegre MC, et al. Antimicrobial resistance of Gram negative bacilli isolated from terciary-care hospitals in Colombia. Biomédica. 2010;30:371-81. https://doi.org/10.7705/biomedica.v30i3.271
Fournier PE, Richet H. The epidemiology and control of Acinetobacter baumannii in health care facilities. Clin Infect Dis. 2006;42:692-9. https://doi.org/10.1086/500202
Ovalle MV, Saavedra SY, Rodríguez MK. Informe de resultados de la vigilancia por laboratorio de resistencia antimicrobiana en infecciones asociadas a la atención en salud. Bogotá, D.C.: Instituto Nacional de Salud; 2018.
Ovalle MV, Duarte C, Zambrano C. Informe de resultados de la vigilancia por laboratorio de resistencia antimicrobiana en infecciones asociadas a la atención en salud. Bogotá, D.C.: Instituto Nacional de Salud; 2019.
Ovalle MV, Duarte C, Leal AL, Zambrano C. Informe de resultados de la vigilancia por laboratorio de resistencia antimicrobiana en infecciones asociadas a la atención en salud. Bogotá, D.C.: Instituto Nacional de Salud; 2020.
Ovalle MV, Duarte C, Flórez AC, Leal AL, Zambrano C. Informe de resultados de la vigilancia por laboratorio de resistencia antimicrobiana en infecciones asociadas a la atención en salud. Bogotá, D.C.: Instituto Nacional de Salud; 2021.
Organización Panamericana de la Salud. Reporte de situación COVID-19 Colombia No. 285- 25 de agosto 2022. Fecha de consulta: 20 de agosto del 2023. Disponible en: https://www.paho.org/es/reportes-situacion-covid-19-colombia
Saavedra Trujillo CH. Consenso colombiano de atención, diagnóstico y manejo de la infección por SARS-CoV-2/COVID-19 en establecimientos de atención de la salud. Recomendaciones basadas en consenso de expertos e informadas en la evidencia. Infectio. 2020;24:50-60. https://doi.org/10.22354/in.v24i3.889
Rawson TM, Ming D, Ahmad R, Moore LSP, Holmes AH. Antimicrobial use, drug-resistant infections and COVID-19. Nat Rev Microbiol. 2020;18:409-10. https://doi.org/10.1038/s41579-020-0395-y
Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet. 2020;395:507-513. https://doi.org/10.1016/S0140-6736(20)30211-7
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020;395:1054-62. https://doi.org/10.1016/S0140-6736(20)30566-3
Rawson TM, Moore LSP, Zhu N, Ranganathan N, Skolimowska K, Gilchrist M, et al. Bacterial and fungal coinfection in individuals with coronavirus: A rapid review to support COVID-19 antimicrobial prescribing. Clin Infect Dis. 2020;71:2459-68. https://doi.org/10.1093/cid/ciaa530
Rawson TM, Moore LSP, Castro-Sánchez E, Charani E, Davies F, Satta G, et al. COVID-19 and the potential long-term impact on antimicrobial resistance. J Antimicrob Chemother. 2020;75:1681-4. https://doi.org/10.1093/jac/dkaa194
Thomas GR, Corso A, Pasterán F, Shal J, Sosa A, Pillonetto M, et al. Increased detection of carbapenemase-producing Enterobacterales bacteria in Latin America and the Caribbean during the COVID-19 pandemic. Emerg Infect Dis. 2022;28:1-8. https://doi.org/10.3201/eid2811.220415
Some similar items:
- Nancy Yaneth Flórez , Stefany Alejandra Arévalo , Edna Catering Rodríguez , Jaime Guerrero , Kelly Paola Valverde , Paula Lucía Díaz , Lucy Angeline Montaño, Doris Mabel Gartner , Carolina Duarte , Jaime Enrique Moreno, An outbreak of Salmonella enterica subsp. enterica serovar Give associated with foodborne illness in the department of Vichada, Colombia, 2015 , Biomedica: Vol. 41 No. 1 (2021)
- Alexandra Hurtado-Ortiz, José Moreno-Montoya , Franklyn E. Prieto-Alvarado , Álvaro J. Idrovo, Benchmarking of public health surveillance of COVID-19 in Colombia: First semester , Biomedica: Vol. 40 No. Supl. 2 (2020): SARS-CoV-2 y COVID-19
- Edgar F. Manrique-Hernández, José Moreno-Montoya, Alexandra Hurtado-Ortiz, Franklyn E. Prieto-Alvarado, Álvaro J. Idrovo, Performance of the Colombian surveillance system during the COVID-19 pandemic: A rapid evaluation of the first 50 days , Biomedica: Vol. 40 No. Supl. 2 (2020): SARS-CoV-2 y COVID-19
- Jaime E. Bernal, Martha Lucía Tamayo , Ignacio Briceño , Escilda Benavides , Newborn screening in Colombia: The experience of a private program in Bogotá , Biomedica: Vol. 44 No. 1 (2024)
- Raúl Murillo, Ricardo Cendales, Carolina Wiesner, Marion Piñeros, Sandra Tovar, Effectiveness of cytology-based cervical cancer screening in the Colombian health system , Biomedica: Vol. 29 No. 3 (2009)
- Sandra Lorena Girón, Julio César Mateus, Fabián Méndez, Impact of an open waste disposal site on the occurrence of respiratory symptoms and on health care costs of children , Biomedica: Vol. 29 No. 3 (2009)
- José Joaquín Carvajal, Ligia Inés Moncada, Mauricio Humberto Rodríguez, Ligia del Pilar Pérez, Víctor Alberto Olano, Characterization of Aedes albopictus (Skuse, 1894) (Diptera:Culicidae) larval habitats near the Amazon River in Colombia , Biomedica: Vol. 29 No. 3 (2009)
- Andrés Páez, Gloria Rey, Carlos Agudelo, Alvaro Dulce, Edgar Parra, Hernando Díaz-Granados, Damaris Heredia, Luis Polo, Outbreak of urban rabies transmitted by dogs in Santa Marta, northern Colombia , Biomedica: Vol. 29 No. 3 (2009)
- Patricia Escobar, Katherine Paola Luna, Indira Paola Hernández, César Mauricio Rueda, María Magdalena Zorro, Simon L. Croft, In vitro susceptibility of Trypanosoma cruzi strains from Santander, Colombia, to hexadecylphosphocholine (miltefosine), nifurtimox and benznidazole , Biomedica: Vol. 29 No. 3 (2009)
- Mauricio Beltrán, María Cristina Navas, María Patricia Arbeláez, Jorge Donado, Sergio Jaramillo, Fernando De la Hoz, Cecilia Estrada, Lucía del Pilar Cortés, Amalia de Maldonado, Gloria Rey, Seroprevalence of hepatitis B virus and human immunodeficiency virus infection in a population of multiply-transfused patients in Colombia , Biomedica: Vol. 29 No. 2 (2009)
Copyright (c) 2023 Biomedica

This work is licensed under a Creative Commons Attribution 4.0 International License.
Funding data
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |

























